An Assessment of the Personal and Emotional Barriers to Effective Disaster Response on the Part of Healthcare Professionals
Laura L. Banks, DVM, MPH
Michael E. Richards, MD
Mark B. Shah, MD
Center for Disaster Medicine
University of New Mexico Health Sciences Center
Albuquerque, NM
2006
A printable version of this QR report is available in PDF format.
Any opinions, findings, and conclusions or recommendations expressed in this material are those of the author(s) and do not necessarily reflect the Natural Hazards Center.Citation: Banks, Laura, Michael Richards, and Mark Shah. 2006. An Assessment of the Personal and Emotional Barriers to Effective Disaster Response on the Part of Healthcare Professionals. Quick Response Research Report 188. Boulder, CO: University of Colorado Natural Hazards Center. http://www.colorado.edu/hazards/qr/qr188/qr188.html.
Introduction
The objective of the current study is to determine the personal and emotional barriers experienced by the staff of the hospital system in Stuart, Florida, that affected their ability to provide patient care. The study also aims to capture lessons learned from providing patient care during two back-to-back hurricanes. The current study was funded in part by the Natural Hazards Center (University of Colorado at Boulder). Research activities were reviewed by the University of New Mexico Human Research Review Committee.
Overview of the 2004 hurricanes
The community of Stuart, in southeast Florida’s Martin County, was the point of landfall for Hurricane Frances—and again for Hurricane Jeanne three weeks later—in September of 2004. Both hurricanes made landfall as Category 2-3 storms, causing severe community damage and the loss of power and telephones services.
According to the National Hurricane Center, Hurricane Frances made landfall near the southern end of Hutchinson Island, Florida, at 12:30 a.m. on September 5, 2004. Various measured stations reported sustained winds of up to 85 mph and peak gusts up to 108 mph, with estimated storm surges along the Florida coastal regions of 3 to 8 feet above normal tide levels. Various measuring stations in Florida reported minimum surface pressures of 959.0 mb to 962.8 mb (see Figure 1). In addition, a total of 101 tornadoes were reported in association with Frances, with 23 occurring in Florida. Hurricane Frances was directly responsible for seven deaths (five in Florida), and indirectly responsible for 42 deaths (32 in Florida).
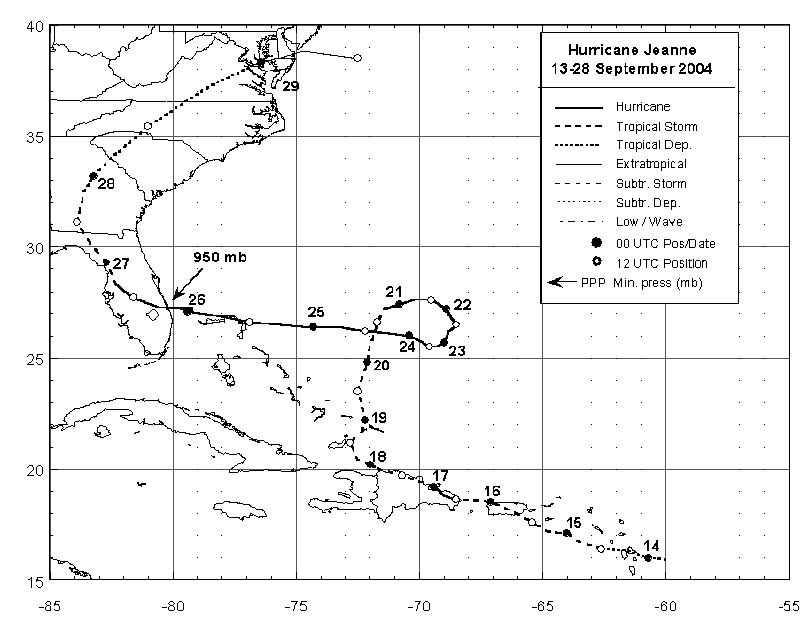
Hurricane Jeanne made landfall on the east coast of Florida, on the southern end of Hutchinson Island and just east of Stuart, at midnight on September 26, 2004. Maximum sustained winds were reported as high as 85 mph, with wind gusts estimated at 121 mph. Maximum surface pressure was estimated to be approximately 950 mb at landfall. Storm surge was estimated to be 3.5 feet to 6.0 feet above normal tide along the coastal regions of Florida (see Figure 2). Hurricane Jeanne was directly responsible for three deaths in Florida.
Martin County, Florida, normally supports two major inpatient hospitals and several satellite facilities, all within Martin Memorial Health Systems (MMHS). MMHS formulated a “Hurricane Procedure Disaster Recovery Plan” in 1993 and revised it in May of 2004. During both hurricane events, the majority of the patients in Martin County were transferred or routed either to Tampa or to Martin County’s more southerly located, smaller hospital due to increased vulnerability of the larger hospital to the north. Hospital evacuation due to the threat of a hurricane is not common—a study of hospital evacuations occurring in the 1990s found that only 14 percent occurred due to hurricanes (Sternberg 2005). Although the majority of the community evacuated the storm area, significant personal injury resulted upon the citizens’ return to their damaged and dangerous homes and businesses. Specific injury information is not available for these events, but a study comparing two hurricanes in 1992 (Andrew and Iniki) found that the most common complaints addressed by federal disaster medical assistance teams (DMATs) during both events were wounds, musculoskeletal pain, medication refills, rash, abdominal complaints, and upper respiratory infections, with 6.3 percent and 4.9 percent of the patients requiring hospitalization during each hurricane, respectively (Nufer 2004). In addition to injuries due to the hurricane and its cleanup, the high volume of day-to-day medical needs of the community reappeared upon the return of the citizenry to Martin County, in spite of the damaged medical care infrastructure. This placed an extreme burden on the hospital system, in the face of decreased hospital capacity.
In the days immediately following Hurricane Frances, DMATs were deployed to the site of the south hospital in Martin County to assist with patient care using a mobile medical center outside the hospital. The practice of deploying DMATs in proximity to hospitals to assist with patient care occurred in other locations in Florida during the 2004 hurricane season (Blaney-Brouse 2004).
Research Methods
The research team conducted a roundtable interview with the management and leadership of the hospital approximately two months after the hurricanes of 2004. The interview was tape-recorded with the permission of the interviewees, using a clearly visible tape recorder located on the meeting room table. Included in the interview were the chief operating officers, the heads of emergency services for both hospitals, and unit managers representing the following departments: surgery, imaging, laboratory services, nutrition services, environmental services, security, and pastoral services. Interviews covered topics such as the hospital’s emergency plan as it stood before, during, and after the hurricanes and changes made to the plan; housing of employees and their families; communication with employees and the media during the hurricanes; distribution and scheduling of staff; utilization of the Disaster Service Center made available to the employees; psychological and emotional issues associated with the trauma experienced by the staff; and aggregate data related to services provided to patients during the hurricanes. Also, the hospital management was asked to provide comments on the presence of the three FEMA disaster medical assistance teams that assisted the hospital with patient care after the hurricanes via the mobile field hospital located outside of the south hospital.
In addition, a two-page, written survey created by the research team was distributed, with the assistance of the director of emergency services, to a convenience sample of south hospital emergency services staff, irrespective of their duties during the hurricanes. The survey instrument included queries regarding the regular occupation and duties of the respondent as well as hurricane-related duty assignments; demographic, housing, and family information; and the presence or absence of various hurricane-related challenges, barriers, and services offered.
Lessons learned
The leadership of MMHS was extremely proud of its staff’s dedication during the hurricane season of 2004 and welcomed the opportunity to review the MMHS response to the challenges that arose. The outcome of the roundtable discussions are summarized below into categories that address common themes.
General operations
During the hurricanes, many in the community wanted to go to the hospital as a “shelter,” in spite of the fact that the hospital needed to decrease the number of patients. In addition, loss of critical referral units, like the mental health holding unit, resulted in the hospital keeping those patients, further adding to the hospital census. During the response to the hurricanes, the north hospital in the system used a modified Incident Command System, whereas the south hospital did not.
The MMHS pharmacy was very active after the storms and required additional staffing. Emergency supplies came on pallets from suppliers. All pharmaceuticals were distributed to individual patients out of the hospital pharmacy, even if prescribed by DMAT physicians. This procedure was used, rather than distributing medication to the DMAT mobile hospital, so that the drugs could be logged for later reimbursement.
As soon as possible after the storms, a labor pool was created and organized by the staffing office. Employees without ongoing duties, predominantly from the closed satellite facilities, were asked to call in and give their availabilities for work. Staff from the labor pool was used outside of regular duties for response and recovery, and the staffing office restructured duties to keep people working. By using a labor pool, MMHS was able to give temporary jobs to its employees who would otherwise be temporarily unemployed. In addition, MMHS felt it was important to present a public image that the hospital was functional and “in control” by using the labor pool to quickly remove debris from the hospital grounds and to assist in minor repairs. Associates were paid their regular rate of pay, no matter what their duties. MMHS administration and staff both felt that use of the labor pool greatly sped the recovery of the facility and boosted the morale of the employees.
Planning
Healthcare system planning must anticipate increased needs. In general, the MMHS response plan included suspension of some activities and shunting of staff from outlying facilities. All employees were required to choose either the “A-Team” (to work just before and during the storm) or the “B-Team” (to work after the storm passed and travel was safe) as part of their employment; the hospital then filled the needs at the time of the hurricane. Employees were made aware that their duties might change during an emergency.
Healthcare system plans should include procedures to either provide additional staff, or shunt staff by temporarily shutting down unneeded satellite facilities. Plans should also include procedures to systematically shut down vital equipment prior to loss of power, as well as department-specific plans to deal with power outages. Hospitals should consider shared credentials and drills, and including satellite facilities in their plans.
Staffing
Healthcare workers have historically been a vital part of disaster response. One of the first publications on this subject outlined the important role of public health nurses immediately following the 1925 tornado in southern Illinois (MacMaster 1999). During the 2004 hurricanes in Florida, it was important to keep people working, doing something, staying engaged in the organization, and most importantly, getting paid in order to help offset personal challenges. Three “types” of employees emerged:
- Those who were able and willing to stay and perform any task;
- Those who left immediately; and
- The in-between group who stayed in the community but were unable or unwilling to take on expanded duties.
This variation in willingness or ability to perform assigned duties was similar to that described by French following Hurricane Floyd in 1999 (French 2002). The second storm in 2004 (Jeanne) resulted in more community damage, and employees were increasingly torn between home and work. For the most part, however, the MMHS employees were very willing to do whatever was needed.
During the first hurricane, MMHS realized that more clear instructions were needed for the A- and B-Teams. Instructions needed to be specific regarding the duties required—tasks were then specifically assigned and not left to chance. The hospital set up criteria for positions based on skills mix. In addition, the B-Team was given more clear direction regarding the required commitment and the communication methods that would be used to notify staff when to come in to work. For Hurricane Frances, the B-Team was asked to report to work when notified. These notifications came in the form of television, radio, and phone calls. However, due to decreased communication capability, there was a large variation in when B-Team members could be reached and when they consequently arrived at the facility to relieve A-Team members, some of whom had been working for 36 or more hours. In contrast, for Hurricane Jeanne, the B-Team was asked to report for duty based on publicized wind speed decreases, rather than at a specific time or due to a specific call-out. This greatly decreased the variation in B-Team member arrival at the facility.
For Hurricane Jeanne, the A-Team was scaled down because of the relative lack of in-hospital patients during the storm. Unfortunately, this decrease resulted in individual services within the health system (e.g., laboratory services and radiology) experiencing serious staff shortages when patients returned after the storm, ahead of the employees.
Hospitals must also identify key players and provide cross-training. This includes power plant operators and other non-clinical staff. In addition, key equipment must be identified (e.g., the MMHS south hospital did not normally keep OB/GYN equipment). MMHS was very fortunate that some staff from the north and south hospitals, as well as the satellite facilities, were cross-trained as part of the hospital system.
Communication
The damaged community infrastructure during the storms (lack of electricity and telephone service, and damage to the local newspaper publisher) made communication with employees difficult. Employees were encouraged to have battery-powered radios, and were informed as to which stations to listen to. When telephone services were available, managers left department-specific messages for their employees on voicemail and provided a “Hurricane Hotline” telephone number for employees. MMHS had a daily “hot sheet” distributed to employees in the whole hospital system. These techniques used to communicate with staff were similar to those described by McCaughrin in response to the catastrophic flooding caused by Hurricane Allison in Houston (McCaughrin 2003). Regarding media coverage, it was challenging to get Stuart community information into the West Palm Beach-centered media, but there was improved responsiveness during Hurricane Jeanne, including messages specifically targeted to hospital employees. This technique has been established elsewhere in the United States, including by Houston’s St. Luke Episcopal Hospital (Neil 2003). External communication was also improved during the second storm, with the Martin County Emergency Operations Center tracking what medical supplies were available in the county and helping to notify the community about which healthcare facilities were open.
Special Services
As in any community-wide emergency, the MMHS employees were concerned for the safety of their families. Family members of employees were allowed to seek shelter at the hospital during the storms, provided that they were pre-identified, registered, and wearing a wristband. During Hurricane Jeanne, MMHS was forced to restrict the definition of “family” in order to decrease the number of people that required resources and space in the facility. Family members who wanted to volunteer with hospital duties were put into the labor pool. Members of the labor pool provided child care while families were housed within the hospital.
During the storms, the local humane society provided care for the pets of first responders and for rescued animals, but quickly became overwhelmed. MMHS realized the need to provide pet care for employees, and added pet care services for Hurricane Jeanne. In total, 26 dogs and 7 cats were cared for by 14 labor pool employees at the fitness center.
Food services were provided free to the public and to hospital employees during and after Hurricane Frances, with 17,000 meals served. This service was difficult to maintain, and was not offered to the public during Hurricane Jeanne.
Recovery
MMHS utilized an employee Disaster Resource Center modeled after Lee Memorial Center in Fort Myers, Florida. The center assisted 615 employees by providing information on the availability of supplies (such as ice and water), county services, FEMA contacts, internet and telephone service, and emergency housing information. Labor pool employees were used within the Disaster Resource Center by acting as “Disaster Guides.” After the discontinuation of the labor pool, the “Disaster Guides” were limited to human resources employees.
Prior to the storms of 2004, MMHS developed the “Associate Disaster Relief Fund” to provide financial assistance to employees during community disasters. The sources of funds included employee fundraisers, employee donations, foundation and commercial donations, and matching MMHS funds. The fund distributed over $146,000 of disaster relief to employees during the 2004 hurricane season. A similar fund was established for hospital staff during the response to Hurricane Allison flooding in Houston (McCaughrin 2003). In addition to the financial assistance, an informal “sharing” mechanism developed at MMHS in which employees shared resources.
In order to care for the psychological and emotional needs of the employees, a “Health and Healing Team” was available and visited various hospital departments to provide information about the service. There was also information about the service on the employee intranet Web site and the daily “hot sheet.” The “Health and Healing Team,” through the employee assistance services, conducted training for employees to enable them to provide counseling for others.
Coordination with federal disaster medical assistance teams
The MMHS leadership made the decision to request DMAT assistance at the most functional hospital in their system at the time—the south hospital—to create the best support system for the community. Two teams were deployed to Stuart during the 2004 hurricanes: NM-DMAT-1 and FL-NM-1.
During the hurricane response, all patients were seen first at the hospital, then triaged to the DMAT mobile hospital adjacent to the hospital if needed. As the hospital staff became more comfortable with the relatively high level of care available in the DMAT tent, they were able to refer patients with more severe needs.
The emotional stress levels of the employees of MMHS were peaking during the second week of the second storm. It was very important to have the psychological boost of the DMAT. The DMAT conducted daily psychological debriefings that were very helpful and resulted in the hospital getting their own psychologist/counselor. It was noted that the physical proximity of the DMAT (in the parking lot) was a huge emotional boost, versus having the teams located somewhere else in the county. The presence of the DMAT allowed the emergency medical staff, which existed in too few numbers to allow significant shift rotations, to attend to some home duties related to the storms.
Logistically, it was noted that hospitals that operate in disaster-prone areas should have outdoor sources of water and power to allow for the operation of mobile, auxiliary, or surge medical services. Also, specific communication was needed to facilitate the local pharmacy’s acceptance of the prescriptions being written by the DMAT physicians. It was also noted that FEMA should have available a description of what services a DMAT can offer to a healthcare system during a crisis to help management decide whether or not their system can utilize a team. MMHS had questions regarding the hospital’s needed commitment, what procedural changes would be required, and what costs would be incurred.
Survey Results
During the week following the research visit, a total of 22 surveys were completed, collected by the director of emergency services, and returned by mail to the research team. Several questions required separate answers for each hurricane and the responses were tabulated for each hurricane and for both hurricanes together, resulting in more than 22 responses to some questions. Research staff recorded the survey results in an electronic spreadsheet to allow for aggregate review. The survey questions relating to the personal and emotional barriers that may have arisen during the hurricane response are included in this report.
Respondents to the survey included personnel who listed their job or profession as physician (6), registered nurse (11), EMS/EMT (1), pharmacist (1), and patient care technical staff (3). Fifteen of the respondents were full-time, regular employees of the hospital, with the remainder being part-time or associated staff. The age range of the respondents was 25 to 56 years of age. Four of the respondents indicated that they lived alone; 18 indicated that they lived with a spouse, child, other family member, or roommate; and 10 owned pets. Ten respondents lived more than 10 miles from the hospital.
Despite the use of pre-disaster training and drills by the hospital, a large minority of respondents (8 out of 22) stated that they did not recall receiving any disaster-related training, while a majority (16 out of 22) stated that they did not recall participating in a drill.
Two survey questions related to the interaction of the hospital staff with the federal DMAT teams, using a visual analog scale of impact. Every respondent indicated at the highest level on the scale (+3) that the DMAT positively affected their ability to provide patient care during the hurricanes. Every respondent indicated that the DMAT had a positive impact on their emotional well-being during the hurricane response, with 19 respondents indicating the highest level of positive impact on the scale (+3).
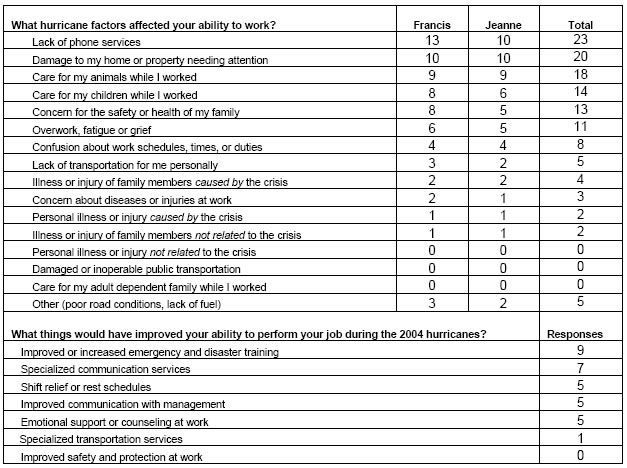
Two survey questions related to the effect of the hurricanes on the employee’s ability to function during the response period, and asked what factors could have improved the response. The results are summarized in Table 1. Improved or increased disaster or emergency training was the most commonly cited item that would have improved the employee’s ability to respond. The most commonly noted factors that affected the employee’s ability to work during the hurricanes were lack of telephone services and damage to the employee’s home or property. Concerns about family, however, were also very important in the employee’s ability to work during the hurricanes. Although MMHS allowed family members to seek shelter at the hospital, none of the respondents in this survey indicated the use of hospital-provided childcare. The concern about family safety correlates to the responses given by Florida nurses in a survey following Hurricane Floyd, in which family and pet safety were considered of primary importance (French 2002).
Conclusions
Disasters affect healthcare infrastructure and delivery in multiple ways. Healthcare systems can mitigate the effects of disasters by developing ways to better utilize their healthcare providers and other staff. There are many physical and emotional barriers that interfere with the ability of staff to come to work in a disaster setting.
We have outlined the ways that Martin Memorial Health System dealt with Hurricanes Frances and Jeanne in September of 2004. Associates did reflect that despite some planning and preparation, even more is needed and viewed as beneficial by survey respondents. Staffing innovations at MMHS included pre-planning for satellite facility closures, partial patient evacuation, the development of disaster teams to meet the hospital’s needs both during and immediately following the disaster, the development of a labor pool, the provision of shelter to families and pets, and improved communication techniques to ensure that associates were informed and able to access assistance. In addition, by enlisting the aid of federal assistance teams, the hospital wass able to further improve the ability of its own staff to perform and speed up the recovery of their healthcare system.
References
Blaney-Brouse D. 2005. Meeting the challenge: First person accounts of Florida nurses’ courageous response to the hurricanes of the Fall of 2004. Journal of Emergency Nursing; 31 (1): 28–33.
French E. 2002. Comparison of Nurses’ needs/concerns and hospital disaster plans following Florida’s Hurricane Floyd. Journal of Emergency Nursing; 28 (2): 111–117.
MacMaster J. 1999. The public health nurse in tornado relief. Public Health Nursing; 16 (1): 72–75.
McCaughrin W. 2003. Perfect storm: Organizational management of patient care under natural disaster conditions. Journal of Healthcare Management; 48 (5): 295–308.
Neil R. 2003. Power of people—part four. Materials Management in Health Care; October: 25–28.
Nufer K.E. and G. Wilson-Ramirez. 2004. A comparison of patient needs following two hurricanes. Prehospital and Disaster Medicine; 19 (1): 146–149.
Sternberg E., G.C. Lee, and D. Huard. 2004. Counting crises: US hospital evacuations, 1971–1999. Prehospital and Disaster Medicine; 19 (2): 150–157.
Figure 1. Best track positions for Hurricane Frances, August 25-September 8, 2004.
(Source: National Hurricane Center)
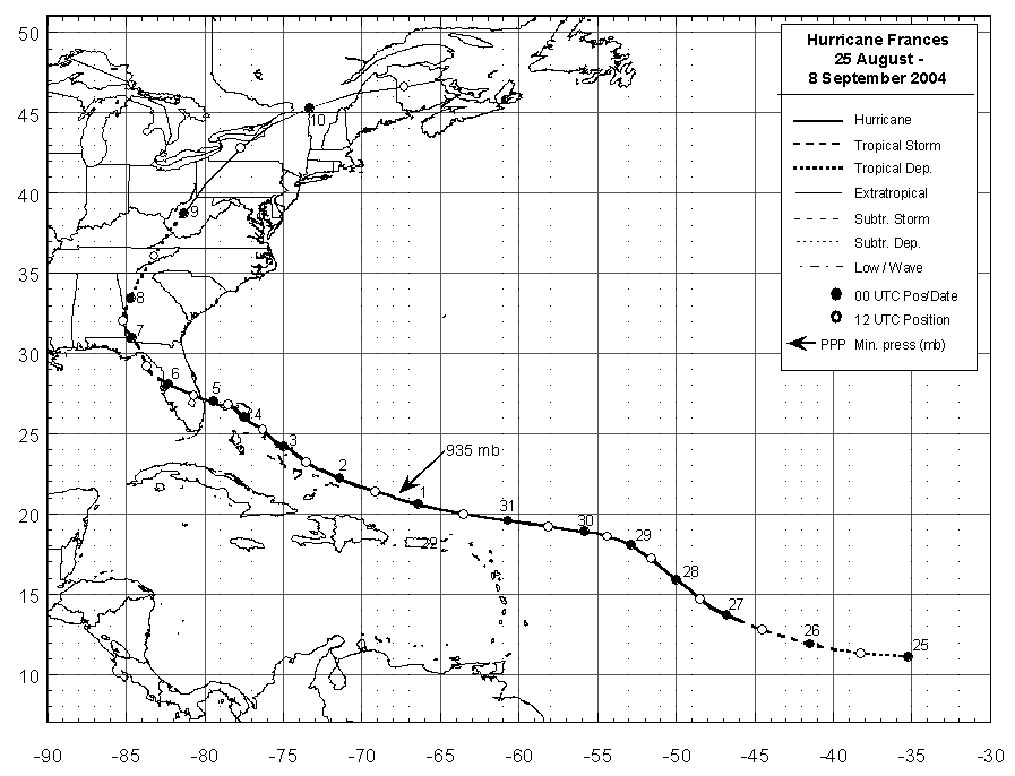
Figure 2. Best track positions for Hurricane Jeanne, September 13-28, 2004.
(Source: National Hurricane Center)
Table 1. Selected survey questions and responses