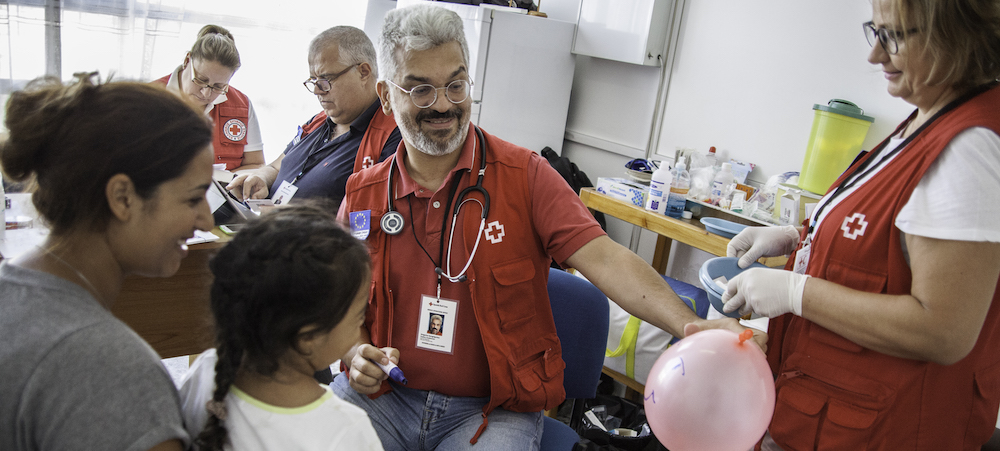
 Shelter workers are called on to provide many different services, including medical care and mental health support. ©Spanish Red Cross, 2016.
Shelter workers are called on to provide many different services, including medical care and mental health support. ©Spanish Red Cross, 2016.
By Tener Goodwin Veenema and Mary Casey-Lockyer
Implications for Public Health
Health outcomes in emergency shelters can be improved by creating systems for disease control, medication management, mental health services, and communication among providers before disasters strike.
Emergency shelters regularly provide services to at-risk populations. These groups—including children, older adults, those experiencing homelessness, and those who are poor or chronically ill—are often disproportionately impacted by disaster. Relocation to a shelter environment can further affect their physical, mental, and emotional well-being.
The interplay of poverty, long-standing health conditions, and psychological trauma creates further layers of vulnerability that can result in poor outcomes for those impacted by disaster. For example, following recent major hurricanes, many shelter residents had high rates of chronic disease, often lacked health insurance, and received some type of public assistance. The burden of chronic disease among shelter populations—compounded by stress, anxiety, grief, and sleeplessness—contributes to the challenges of delivering healthcare services to clients residing in disaster shelters.
For these and many other reasons, healthcare professionals and shelter managers provide healthcare services that can range from basic first aid to advanced chronic disease management. Planning in advance to support healthcare workers and ensure robust healthcare service provision can make all the difference in disasters.
How Healthcare Provision Varies Across Shelters
The American Red Cross (ARC) is designated in the U.S. National Response Framework under Emergency Support Function 6 (ESF-6) as the support agency for mass care and sheltering. As part of a congressional mandate to provide sheltering after disasters and other major events, ARC operates approximately 60% of all disaster shelters in the United States with support from the Federal Emergency Management Agency. The other 40% of shelters are run by a complex mix of non-governmental and faith-based organizations, as well as local and state providers.
After large scale events, shelters often serve as satellite healthcare settings that function outside of the normal regulatory oversight of the U.S. healthcare system. Because of this, and because of a lack of consistency in shelter operator processes and procedures, the quality of healthcare services can vary from shelter to shelter. Some shelters might be staffed by federal disaster medical assistance teams, while others might rely on volunteers and retired registered nurses, resulting in variability in the scope and types of healthcare services offered.
Research on Promoting Health in Shelters
Our research team conducted an integrative review of published papers and shelter reports to find out what factors were associated with promoting the best health outcomes in shelter populations. Notably, we found that systematic analysis of the quality of health services rendered in disaster shelters is underrepresented in the literature and the true health outcomes of disaster shelter residents are currently unknown.
This is problematic because many disaster victims arrive in need of medications for a range of chronic and acute healthcare needs. In high-population shelters, it is critical that individuals are systematically assessed and tracked by licensed healthcare providers knowledgeable about public health in order to prevent disease outbreaks. Moreover, writing and filling prescriptions requires systems to be in place for medication procurement and distribution. Infection control and prevention measures, such as surveillance, detection, isolation, and quarantine, are crucial for promoting health and so also need to be in place. In addition, the need for mental health services also suggests that the presence of mental health professionals on site would improve quality and completeness of care.
The Centers for Disease Control and Prevention has guidance documents specific to disaster relief for healthcare professionals, as well as a surveillance reporting system and a tool for conducting disaster shelter assessments. Cot-to-cot assessment and surveillance interviews identify possible disease outbreak situations and shelter residents in need of care or referral. The presence of systems to ensure clear and ongoing communication between providers and healthcare organizations about shelter clients and public health reporting can improve overall health and wellness. Finally, our research revealed that identifying a sufficient number of qualified, disaster-trained individuals before an event can ensure that the best healthcare providers and shelter staff are available to support diverse and at-risk shelter populations.
The Takeaway
Our study findings suggest that adequate healthcare staffing levels and staff preparedness; access to medications and medication management; rigorous infection assessment and control programs; timely referrals; bi-directional communication; and access to mental health services are vital to enhancing disaster healthcare services. Most importantly, better pre-event planning and robust preparation for service provision could improve health outcomes, especially among the most at-risk populations, in disaster shelters.
Suggested Tools
Aggregate Morbidity Report Form
Centers for Disease Control and Prevention
This form allows medical staff to conduct active surveillance in shelters during a disaster. The form contains sections pertaining to specific infectious conditions, chronic conditions, mental health, injuries, and routine health maintenance.
Environmental Health Assessment Form for Shelters
Centers for Disease Control and Prevention
A rapid assessment form of shelter conditions to identify immediate public health threats and their sources during a disaster.
For a list of all the tools included in this special collection, visit the Mass Sheltering Tool Index. A list of further readings are also available.

Tener Goodwin Veenema is a professor of nursing at the Johns Hopkins School of Nursing and in the department of international health at the Johns Hopkins Bloomberg School of Public Health. She is an internationally recognized expert in disaster nursing and public health emergency preparedness. Her research is directed toward informing policy related to public health emergency preparedness and response for catastrophic events.