Public Health Implications of 911 Calls During Heat and Smoke Events
Publication Date: 2024
Abstract
Acute climate hazards such as high temperatures and poor air quality can have disproportionate public health impacts on vulnerable populations. Most of the existing literature in this area explores how these hazards affect urban areas, leaving a gap in knowledge about the effects on rural populations and, importantly, how empirical evidence can inform public health emergency preparedness and planning. This study explores the relationship between high temperatures, poor air quality, certain demographic characteristics, and 911 calls in Missoula County, Montana. Employing statistical and geospatial analysis of secondary data, we seek to understand if there is an association between 911 calls, geography, and acute climate events in rural areas and whether these same 911 calls are correlated with vulnerable populations. We also explore the implications of the results for equitable disaster preparedness policy and practice. Findings indicate that as the daily mean temperature rises, 911 calls per 1,000 people increase in census block groups with certain socio-demographic characteristics. Findings suggest strategies that target specific audiences may help improve equity in public health emergency outcomes. For example, focusing heat-related mitigation strategies on communities with many people who are over the age of 65 and/or unemployed or retired.
Introduction
Previous research indicates that acute climate hazards like extreme temperatures and air pollution caused by wildfire smoke events can have disproportionate public health impacts on vulnerable populations (Campbell et al., 20231). Most of the extant literature in this area explores the impacts of acute climate hazards in urban areas and regions outside the United States. (Caulkins et al., 20162), leaving a gap in knowledge about the effects of these hazards on rural populations (Wang et al., 20213). Little work explores how rural geographies with limited adaptive capacity successfully respond and build resiliency to climate hazards (Austin et al., 20214; Lal et al., 20115). Further, certain rural subpopulations (e.g., racial or ethnic minorities) have worse health outcomes than their urban peers (Olshansky et al., 20126). As rural communities are often less resourced (Jerolleman, 20207) and more susceptible to natural hazards (Manuele & Haggerty, 20228), understanding the potential for disparate health impacts from heat and poor air quality events is essential to fostering equitable public health disaster outcomes for rural communities.
This community-engaged multi-disciplinary study explores three interrelated research questions related to the prevalence of 911 calls, geography, socio-demographic characteristics, and acute heat and poor air quality events. By exploring the relationship between 911 calls, geospatial location, demographic factors known to contribute to health vulnerability, and two types of acute climate hazards in one intermountain west U.S. county, findings from this study will contribute to the knowledge on rural vulnerability to climate events as well as equitable public health disaster preparedness and response.
This study is rooted in established practitioner-academic relationships in the community. The research questions at the heart of the study emerged from discussions between the researchers and local public health and emergency managers who were concerned about inequity in public health emergency outcomes in our community. By augmenting community disaster preparedness and planning capacity, we contribute to the resiliency of our local community to future climate hazards.
Literature Review
Climate change poses serious threats to human health (Moulton & Schramm, 20179); these negative health impacts of a changing climate are becoming more recognized and apparent (Mahmood & Guinto, 202210). As a result, public health practitioners, policymakers, and emergency managers are increasingly focused on developing and implementing strategies for improved response to environmental public health disaster events, like heat waves (Bassil et al., 200811). Acute climate hazards affect all populations in some way, yet not all groups are equally at risk (Portier et al., 201312; Reid et al., 201913).
Previous literature suggests that factors such as age (Conti et al., 200514), income (Lim & Skidmore, 202015), level of education (Medina-Ramon et al., 200616), and household configuration (e.g., single parents) (Klinenberg, 201517) contribute to increased vulnerability during high heat. Specifically, there is growing interest in “identifying individual and community vulnerability” to heat (Zottarelli et al., 2021, p. 27118), both through academic research, as well as innovative heat-mapping endeavors that can help inform policymaking to reduce vulnerability (e.g., King County Executive, 202119).
Excessive heat can cause an individual to experience cramps, dehydration, fainting, heatstroke, heat exhaustion, disease exacerbation, and ultimately mortality (Lowe et al., 201120). Likewise, wildfire smoke can impair lung function and increase asthma attacks and has been linked to increased risk of heart attack, lung cancer, stroke, and declines in cognitive functions (MacMillian, 202321). High heat and poor air quality affect public health and the delivery of basic services (Weinberger et al., 201822).
Several previous studies investigate the relationship between 911 and/or emergency service calls and environmental health events throughout the world (Alessandrini et al., 201123; Elliot et al., 201624; Ito et al., 201825; Schaffer et al., 201226; Schneider et al., 202327; Li et al., 202128; Zhou et al., 202329), many of which utilize a secondary data analysis methodology. In general, this work considers residents’ calls for and/or use of emergency services as an indicator of the adverse health impacts of an event on the community. Yet, we are unaware of any research that has used its findings to inform public health disaster preparedness and response planning.
Recent research suggests that extreme heat affects the demand for emergency services, including calls for police (Rotton & Cohn, 200430) and emergency medical services (Caulkins et al., 2016). Despite growing evidence regarding the impacts of high heat, poor air quality, and climate change on emergency services, climate action plans rarely identify heat preparedness for emergency services. Local, state, and federal governments must consider not only the impact of heat on socially or medically vulnerable populations but also how those incidents will affect the larger system response (Williams et al., 202031). For rural and remote communities to equitably mitigate and prepare for the health impacts of climate change, it is important to consider the specific local and regional socio-cultural, economic, and geographic contexts (Kipp et al., 201932).
Research Questions
To assist county emergency management and public health units in developing adaptive management strategies (pre-event planning and response), this study uses 911 call data to explore four research questions:
- Does the rate and geographic clustering of emergency 911 calls in Missoula County, Montana, change during acute climate events—specifically, extreme heat and poor air quality events?
- Are 911 calls during acute climate events more likely to come from communities with higher rates of socially vulnerable populations? If so, which types of vulnerable populations were present in the communities that most called 911?
- During poor air quality and extreme temperature events, which geographic locations are most vulnerable to disparate health outcomes as indicated by 911 call frequency?
- Where should disaster preparedness planning be directed to advance equitable public health outcomes?
Research Design
This study employs analysis of secondary data—that is data that were collected for another purpose—to explore novel research questions (Omukuti et al., 202133). Secondary data analysis is a popular method in empirical public health emergency preparedness literature (Yeager et al., 201034), work exploring community disaster recovery and resilience generally (Mayer, 201935), and research designed to guide public health disaster planning specifically (Hope et al., 201036; Leonardi et al., 200637; Lu et al., 200738). Secondary analysis offers researchers the opportunity to analyze preexisting datasets and conserve limited financial resources (Dale et al., 200839).
We elected to use a secondary analysis approach in this research study for several reasons. First, this study was funded by the Natural Hazards Center’s Public Health Disaster Research Award Program (with the Centers for Disease Control and Prevention and the National Science Foundation) which prioritizes research that is rapid. By using existing data, we set out to answer critical questions related to both recent and anticipated climate disasters in Missoula County on an expedited timeline.
Second, our approach aligns with the priorities of convergence-oriented research. The genesis of this study is rooted in a “specific and compelling problem” identified by the Missoula County Office of Emergency Management and Missoula City-County Health Department (Peek et al., 2020, p. 240). Specifically, Missoula County leaders suspected that the number of 911 calls increased during days with extreme temperatures or poor air quality. They also thought that those calls may be originating from communities with higher rates of social vulnerability. In fact, previous efforts to conduct this investigation failed to be realized due to lack of funding dedicated to supporting the project. In this study, we set out to provide evidence as to whether heat and poor air quality events were linked to increased 911 calls and illuminate how Missoula County can direct pre-disaster interventions to ensure more equitable public health outcomes.
Study Site and Access
Missoula County, Montana, covers approximately 2,600 square miles and is home to nearly 120,000 people. Within the county, the City of Missoula (population 76,995) is the only incorporated community, meaning approximately one-third of county residents live in small unincorporated towns or rural areas (Missoula County, n.d.-a41, n.d.-b42). There are several vulnerable groups in Missoula County, including residents living in poverty, families who lack adequate emotional and/or social support, veterans, people with disabilities, immigrant and refugee populations, and adults over the age of 65, among others (Missoula City-County Health Department, 201243; U.S. Census Bureau, n.d.-a44). We also classified as vulnerable those residents who are unhoused or under-housed—defined here as anyone lacking access to safe, secure, and affordable housing. The definition also includes those in housing units that are too small for the household composition (Bernstein, 201345).
Several factors make Missoula County, located in western Montana, highly susceptible to poor air quality: the mountain valley topography, widespread dependence on woodstoves to heat homes, and climate change (Therriault & Schmidt, 200146). While several programs have successfully improved air quality in the region, climate change contributes to the increased length and severity of the area’s wildfire season (Missoula County, n.d.47). Projections also indicate that Missoula County is likely to experience “hotter, drier summers; warmer, wetter springs; decreased low-elevation snowpack, and earlier spring runoff” (Maneta et al., 2019, p. 348). Over the next 20-30 years, Missoula County is projected to experience an increase in mean air temperatures of two-to-five degrees Fahrenheit (Cilimburg et al., n.d.49). The impacts of a warming climate and air quality are interrelated as increased heat and drought in the region lead to more wildfires and wildfire smoke (Maneta et al., 2019).
Additionally, Missoula County is predicted to experience “more frequent and intense wildfires…and more wildfire smoke” (Maneta et al., 2020, p. ES-150). Poor air quality increases the likelihood that residents will develop chronic obstructive lung disease (COPD), chronic bronchitis, cardiovascular disease, and/or lung cancer (Minnesota Pollution Control Agency, n.d.51). Those most likely to be impacted include older adults, children under 18, pregnant people, outdoor workers, and low-income individuals (Environmental Protection Agency, n.d.-a52). Likewise, wildfire smoke can impair lung function and increase asthma attacks and has been linked to increased risk of heart attack, lung cancer, stroke, and declines in cognitive function (MacMillian, 2023).
This project emerged from an organic opportunity whereby emergency management and public health leaders identified the desire to undertake an investigation of the variables under study but lacked the resources and capacity to do so. This collaborative research process helps to establish trustworthiness and relevance of the research and is well-equipped to explore questions related to equity and justice within a community (Worden et al., 202253).
Secondary Data
As outlined in Table 1, this project combines secondary data from the American Community Survey (U.S. Census Bureau, n.d.-b54), the Missoula County Office of Emergency Management, and the University of Montana’s Center for Population Health Research. (Table A1 in the Appendix provides full citations for each data set we used in the study). Regarding the 911 call data, it is publicly available on the Missoula City-County website, as described in the Appendix, but our project partners at the Missoula County Office of Emergency Management provided it to us as Microsoft Excel exports, one for each month under study. The Excel files included call date and time, call identification number, call type, incident latitude and longitude coordinates, and an indication of which municipal office or resource (e.g., municipal firefighters, local police, ambulance, etc.) responded to the incident. Air quality and temperature data provided by Center for Population Health Research were sourced from Landguth et al. (2022)55 and the Northwest Alliance for Computational Science and Engineering PRISM Climate Group (2024)56.
Table 1. Study Variables and Data Source
| 911 Calls in 2020 | Missoula County Office of Emergency Management |
| Temperature | Center for Population Health Research |
| Air Quality (PM 2.5) | Center for Population Health Research |
| Nonwhite Resident | American Community Survey |
| Households Receiving Public Assistance | American Community Survey |
| Average Household Income | American Community Survey |
| High School Education or Less | American Community Survey |
| Renter-Occupied Households | American Community Survey |
| Households With Annual Income Under $50,000 | American Community Survey |
| Unemployed or Not in the Labor Force | American Community Survey |
| Adults Over 65 | American Community Survey |
All data were grouped at the census block group level, which is a statistical division of census tracts that typically contains between 600 to 3,000 people (U.S. Census Bureau, 201057). Data retrieved from the American Community Survey were reported as the percentage of the block group population that held the characteristic (e.g., percentage of block group that are over the age of 65).
Dependent Variable
We used 911 calls in Missoula County, Montana, during 2020 as the dependent variable. There were 101,163 in 2020, a decrease of 7,023 calls compared to the previous year, some of which may be attributable to the COVID-19 pandemic; however, as displayed in Table A2 in the Appendix, 911 calls in Missoula County have been declining year over year since 2017. For the purpose of this study, we included all 911 call data in our analysis and did not limit our analysis by call type. Prior studies (e.g., Wang et al., 2021, Williams et al., 2020) of acute climate hazards and public health outcomes have used a similar approach with aggregate secondary datasets of ambulance calls, aggressive behaviors, traffic accidents, and violent crime.
We created two versions of the dependent variable. The first was a raw measure of average 911 calls per day in Missoula County per census group block. Since population size in Missoula County’s census block groups varies from 455 residents and 3,647 residents, however, we recognized that this variation could affect the raw propensity of 911 calls per day. To hold population constant, we created a second normalized measure of 911 calls per day per 1,000 residents by census block group. This allows us to see which areas require a higher degree of attention and resources than would be expected given the population. The raw and standardized measures were highly correlated (0.91, as described in more detail below) and produced similar results across all statistical tests.
Independent Variables
Independent variables fell into two categories: (1) climate events including heat and poor air quality, and (2) socioeconomic characteristics typically associated with population vulnerability.
Regarding climate events, we first measure temperature in units of degrees Celsius. Missoula County expects to experience hotter, drier summers which are anticipated to have intense impacts on public health outcomes for area residents (Maneta et al., 2020). Because of this forecasting, community organizations are actively engaged in planning efforts around mitigating the impacts of extreme heat in the County. While cold temperatures could also indicate events leading to a higher incidence of 911 calls, for the purpose of this study, we focus solely on heat by limiting our data sample from June 1, 2020 to October 15, 2020 which is typically the warmest period of the year in Missoula County (National Weather Service, n.d.58) and aligns with ongoing community planning efforts.
To identify poor air quality events, we used particulate matter (PM) 2.5. PM, which is sometimes called particle pollution and indicates the mixture of solid particles and liquid droplets found in the air that are small particulate matter (diameters of 2.5 micrometers or less). These fine, inhalable particles pose the greatest risk to health and PM2.5 is a common measure used for evaluating air quality (Environmental Protection Agency, n.d.-b59). The second category of independent variables consisted of socioeconomic variables that were sourced from the American Community Survey (ACS) five-year average and represent mean characteristics of census block groups. The American Community Survey (ACS) five-year estimates included in this study are from the most recent (2018-2022) data. The ACS is a non-overlapping dataset (e.g., 2013-2017 ACS and 2018-2022 ACS), meaning comparisons across time can be made.
Data Analysis Procedures
Data from each source were compiled into a primary file and imported for analysis into Stata 18 and ArcGIS. The primary file treats each day within one census block group as one observation (e.g., January 1, 2020, in Missoula County Census Tract 1.00, Block Group 1). Our preliminary analysis includes data from January 1 to December 14, 2020, translating to 30,363 unique observations across 349 days for all 87 census block groups in Missoula County. (Temperature and PM2.5 data were unavailable December 15-31, 2020.) For the analysis focused on extreme heat and wildfire smoke impacts, we narrowed the dataset to the 11,919 observations between June 1 and October 15, 2020. This date range encompasses the four summer months (June, July, August, and September) plus additional days in October to capture the effect of wildfire smoke being present in the county during that month, according to PM 2.5 data. Notably, increasing temperatures and the number of wildfires over 1,000 acres has more than doubled since 1970 and the “wildfire season” is growing increasingly long across western Montana (Climate Smart Missoula, n.d.60).
Statistical analysis was conducted in Stata 18. Using data from the preliminary analysis and primary file, results were mapped by census block group in ArcGIS. We combined the initial data with a detailed map of Missoula County, adding specific socioeconomic information about each census block group. This approach produces a visual representation of the interplay between climate events, socioeconomic indicators, and 911 call frequency at the census block group level within Missoula County.
To determine the relationships among climate events, socioeconomic indicators, and 911 call frequency, we perform a series of hierarchical linear regression models (HLM). This approach nests each observation (i.e., one day) within a particular census block group, thereby accounting for clustering effects within the data in a more appropriate fashion than ordinary least squares (OLS) regression (Raudenbush & Bryk, 200261).
Ethical Considerations and Researcher Positionality
We employed a community-engaged research approach and worked with our community partners to design the study, collect and analyze data, and report findings. We are also attentive to historic practices of extractive data collection and designed this study with our community, rather than about our community. Working in collaborative ways benefits communities and researchers. Our approach centers the realities and perspectives of community officials who are best positioned to design interventions and improve health equity outcomes.
This study relies entirely on anonymized secondary data, which means it is not classified as human subjects research (Office for Human Research Protections, §46.10462). To confirm our understanding of the Common Rule, we consulted with the University of Montana Institutional Review Board to ensure no additional oversight was required and they provided a determination letter that concurred with our assessment. Additionally, principal investigators for this project maintain current Research, Ethics, and Compliance training status and follow best practices for ethical research. Investigators also completed the CONVERGE training on Public Health Implications of Hazards and Disaster Research Training Module (Hansen et al., 202263). Simply, this project directly supports the efforts of Missoula County emergency management and public health agencies to ameliorate health disparities across vulnerable populations.
Results
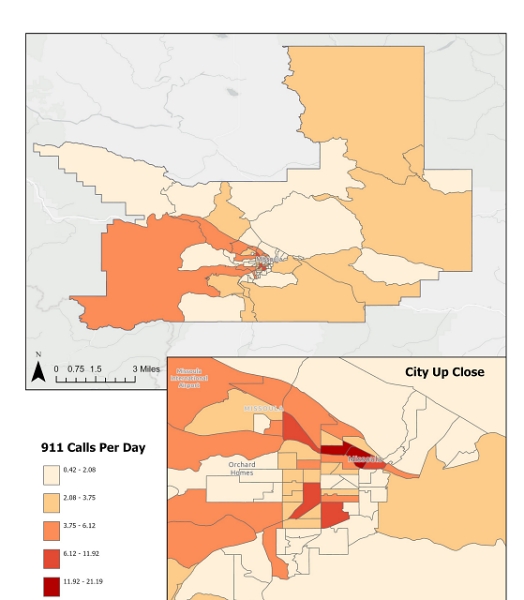
To address our first set of research questions—which concerned the association between emergency 911 calls, geography, and acute climate events in Missoula County, and the relationship of emergency 911 calls during extreme temperature events with vulnerable populations—we began by exploring the raw frequency of 911 calls per day by census block group. Figure 1 depicts the average number of 911 calls per day in 2020 across Missoula County, as delineated by census block group. Darker colors represent higher raw frequencies of 911 calls, while lighter colors depict fewer calls. Initial analyses using HLM determined that approximately 60 percent of the variation in 911 calls per day may be attributed to the census block group level, which indicates that there are relatively predictable patterns of where 911 calls originate from each day. For example, areas that are more urbanized tend to have higher 911 call frequency. This is exemplified in Figure 1, which shows that 911 call frequency from January 1 to December 14, 2020, ranged from 0.4 calls per day in one block group to more than 21 calls per day in another.
Figure 1. Average Raw Number of 911 Calls Per Day by Census Block Group, Missoula County, 2020
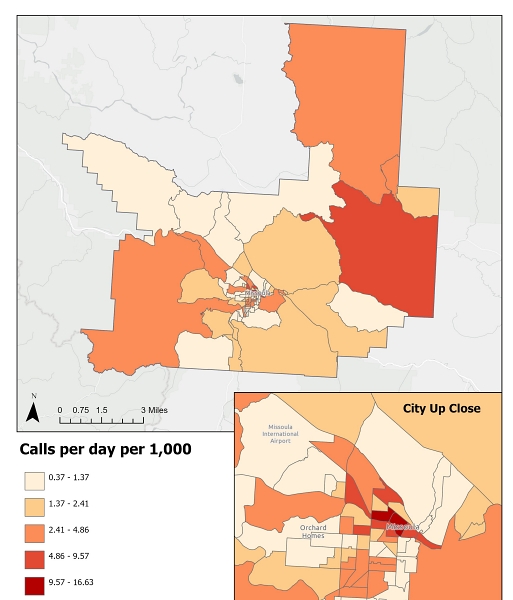
When conducting the analysis using the normalized dependent variable of average 911 calls per day per 1,000 people in each census block group, we find that the mean daily calls was 2.55 across Missoula County, with individual block group averages ranging from 0.37 to 16.63 calls per day per thousand people (see Figure 2). This analysis shows that the rate of people calling 911 in some more urban census block groups within the City of Missoula was lower than the rate in some rural census block groups outside the City limits. Figure 2 shows, for example, a relatively larger call volume in the rural northern and eastern segments of the county. Even though there may be fewer people living in rural areas overall, our analysis shows an increase in call volume in these areas. This is important for emergency services providers to consider as the deployment of resources and access to certain rural areas may require nuanced planning.
Figure 2. Average 911 Calls Per Day Per 1,000 by Census Block Group, Missoula County, 2020
Given the variation in 911 calls across block groups even after accounting for population size, we next explored whether socioeconomic characteristics may explain some of this disparity. We used a correlation matrix analysis to determine the association between 911 calls per day (raw and per 1,000 residents) and each socioeconomic factor under study. (Full results of the correlation matrix are presented in Table A3 in the appendix.) The analysis showed that economic metrics of a community are strongly related to higher 911 call incidence. In particular, the proportion of households occupied by renters within a census block group was strongly associated with higher 911calls per day, alongside metrics like the proportion of households with annual income under $50,000 and mean income (expressed in dollars). Demographic indicators like race, age, education, and unemployment status were not significantly correlated with 911 call incidence.
To address the set of research questions concerning the geographic locations that are most likely to have disparate health outcomes during extreme climate events, we explored the association between high heat temperature and air quality events and 911 calls over the period of June 1 to October 15, 2020.
Between June 1 and October 15, 911 call frequency was significantly higher than the non-summer months (2.91 calls per day per 1,000 people), indicating that 911 calls in Missoula County increased during the (hot) summer months overall. HLM analysis provides insights into how socioeconomic characteristics of the population in each census block group affected the likelihood of calling 911. The first column in Table 2 shows the effect of each independent variable on daily 911 calls per 1,000 residents within a particular block group. These coefficients represent the change in expected daily 911 calls per 1,000 residents with each one-unit increase in the relevant independent variable (e.g., a change in temperature by one degree Celsius; a one percentage-point increase in the share of non-white residents). The first column shows that on average, an increase in mean daily temperature by one degree Celsius was associated with an additional 0.0286 daily 911 calls per 1,000 people in a block group. This effect was significant at the 0.01 level and was also the strongest effect in the entire model.
Table 2. The Effect of Climate Hazards and Socioeconomic Indicators on Daily 911 Calls per 1,000 Residents People
Main Effects |
Interaction With Percentage of Renters |
Interaction With Percentage of Unemployed |
Interaction With Percentage Over 65 |
|
| Average Temperature (°C) | (5.81) |
(2.23) |
(-0.35) |
(0.77) |
| Average Particulate Matter (PM) | (-1.94) |
|||
| Nonwhite Residents (%) | (-0.02) |
|||
| Households With Public Assistance (%) | (-2.00) |
|||
| Average Income ($) | (0.49) |
|||
| High School Education or Less (%) | (0.70) |
|||
| Households With Income Under $50k (%) | (1.35) |
|||
| Households Occupied by Renters (%) | (2.74) |
(3.82) |
||
| Unemployed or Not in Labor Force (%) | (0.55) |
(-0.08) |
||
| Residents Over 65 (%) | (0.30) |
(-0.86) |
||
| Average Temperature x Percentage of Renters | (1.27) |
|||
| Average Temperature x Percentage Unemployed/Not in Labor Force | (2.37) |
|||
| Average Temperature x Percentage of Residents Over 65 | (2.36) |
While average daily temperature did have a significant impact on daily 911 calls per 1,000 people, particulate matter—our measure of air quality—did not have the same impact. An increase in the average daily PM 2.5 measure was instead associated with slight decreases in the incidence of daily 911 calls per 1,000 residents. Due to this finding, we focused subsequent analyses on the effect of temperature, as opposed to air quality. Of all the socioeconomic indicators in the first column of Table 2, only the share of households occupied by renters was significantly related to a higher incidence of 911 calls when holding all other socioeconomic factors constant.
Finally, to address our final research question—where disaster preparedness planning should be directed to advance equitable public health outcomes—the subsequent columns in Table 2 display select interaction effects to determine whether the impact of temperature on daily 911 calls is stronger in areas with certain demographic characteristics. Each column contains three coefficients, but the coefficient of interest is always furthest at the bottom (i.e., the interaction term coefficient).
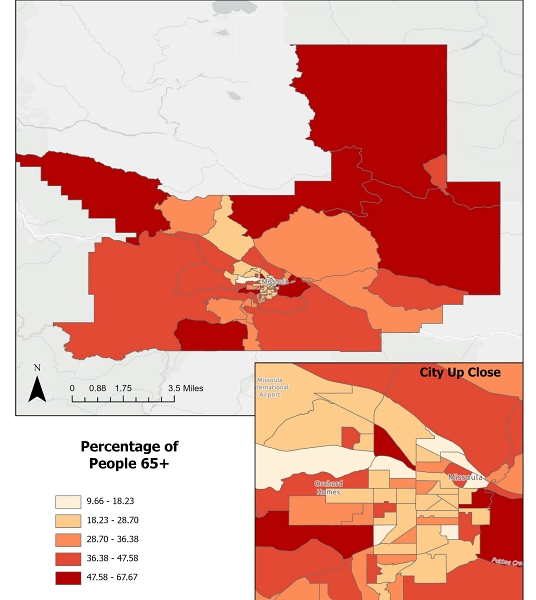
Positive interaction coefficients indicate that the effect of temperature on 911 calls is stronger in areas with higher levels of the indicator involved in the interaction. These interaction effects should help practitioners determine how to deploy resources during a high-heat event, and where emergencies are disproportionately more likely to occur. Our analysis showed that the strongest interaction coefficients were between temperature and two socioeconomic indicators: (1) the share of those who are unemployed or not in the labor force, and (2) the share of residents 65 and over. While both effects are statistically significant, these two variables are strongly correlated (0.73), which could be due to the fact that people over the age of 65 may be retired and therefore counted as not in the workforce. Regardless, as daily mean temperature increases, 911 calls per 1,000 people increase more in block groups with higher levels of these populations. Figure 3 displays the percentage of people who are unemployed or not in the labor force in each of Missoula County’s census block groups. Figure 4 shows the percentage of people aged 65 or over. These figures provide meaningful visual representations of statistical data and map otherwise intangible geography (i.e., census block groups) for greater understanding. Practitioners can use this information to plan for the distribution of resources to areas of the community where people over the age of 65 and those unemployed or not in the labor force are predominantly located.
Figure 3. Percentage of People Unemployed or Not in the Labor Force by Census Block Group
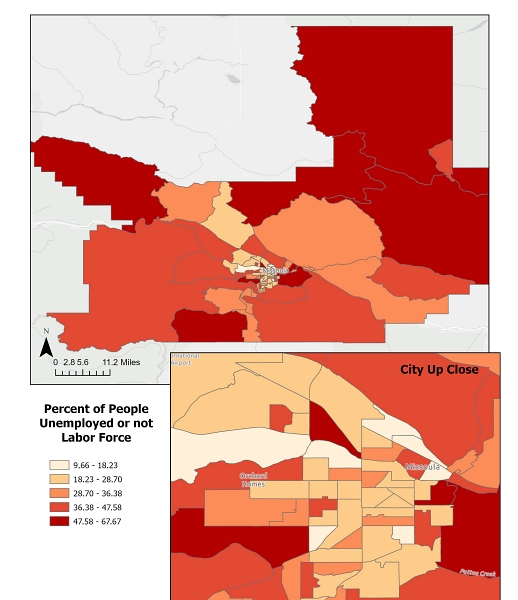
Figure 4. Percentage of Adults 65 Years and Older by Census Block Group
Discussion
The results of this study provide valuable information for Missoula County’s public health emergency planning efforts. First, findings confirm that geographic location accounts for significant variation in daily 911 calls. In total, the study finds that roughly 60% of the variation in daily 911 calls are attributable to geographic location. In other words, 911 calls are not evenly distributed across Missoula County, and certain areas may be more likely to call for emergency services. It is possible that specific geographic features such as highway proximity, adjacency to a river or riparian areas, or tree/greenspace cover may account for some of the variation across the county, but importantly, one implication from this study is that where someone lives explains more than half of the variation in distribution of 911 calls during heat events, and policymakers should incorporate this understanding into future public health planning efforts.
Additionally, findings suggest that during the hottest months of the year, 911 calls increase overall. A month-by-month examination revealed limited spikes in 911 call frequency on particular months or days, and even days where one might expect anomalies (e.g., July 4) did not contain any substantial deviations from the monthly average. Data and time limitations prevent us from fully accounting for factors like increased outdoor activity as confounding effects, though further research could explore this more comprehensively. In fact, with each degree Celsius increase in daily mean temperature, the number of 911 calls rises by 0.03 calls daily per 1,000 people in a census block group, which is roughly a 1% increase in call volume with each additional degree Celsius. This means that if the temperature goes up by ten degrees, the county may expect an approximately 10% increase in call volume per block group.
This study also suggests that significant correlations exist between populations that call 911 frequently and those that possess certain demographic characteristics. Thus, during the hottest days, census block groups that have a larger share of individuals over 65 and unemployed or out of the workforce may have higher rates of 911 calls. This finding is supported by previous research, which suggests that elderly groups, lower-income populations, and unemployed individuals may be more susceptible to health-related issues during heat events for various reasons (for a synopsis, see Bell et al., 202464). Therefore, interventions to increase equity during public health emergencies should be directed to these specific groups.
Finally, this study demonstrates that there could be some census block groups that have both higher rates of 911 calls overall, as well as higher rates of specific socioeconomic characteristics known to contribute to calls for emergency response. However, these groups are not uniform across block groups. The spatial analysis allows us to identify communities where these vulnerable groups are clustered and direct resources for public health emergency preparedness planning to these areas.
Conclusions
Public Health Implications
As a result of this study, local emergency managers now better understand the relationship between heat and increased 911 calls at a more granular level. With increased awareness and understanding, local leaders will be able to use this information to develop mitigation and communication strategies specific to vulnerable populations. The insights from this study will also be shared with local hospitals, clinicians, and emergency services to better prepare for anticipated impacts from adverse heat events.
Further, as area groups undertake long-term public health planning efforts to address increased extreme heat events across Missoula County, attention should be paid to the already stressed cooling capacity of homes, businesses, and other public spaces lacking air conditioning in Missoula County (Cilimburg et al., n.d.49). Anticipated public health impacts from worsening heat and smoke events in Missoula County include premature death, lung cancer, asthma attacks, cardiovascular damage, developmental and reproductive harm (American Lung Association, n.d.65), increases in emergency hospital admissions, acute renal failure, heat exhaustion and heat stroke, among others (Kovats & Koppe, 200566).
Acute mitigation and intervention efforts related to high heat events, such as the deployment of community paramedicine resources, location of cooling shelters, and distribution of other heat-mitigating resources can be directed towards places and groups identified above. Importantly, which preparedness and mitigation tactics and strategies are chosen should be based on the unique demographic profiles across the county, as not all block groups contain the same groups of people. In some cases, county officials may choose to use one intervention to meet the needs of a predominantly older population, but in another area, may choose a different strategy to meet the needs of lower-income individuals. The results of this study provide insights into how to tailor public health preparedness policy and practice to meet the varying needs of different populations.
Limitations
Several limitations are present in this study. First, data included in the analysis reflects a single year (2020), so findings might be influenced by several factors, including the COVID-19 pandemic. (See, for instance, Abrams, 202167; Ashby, 202068; Bowman & Gallupe, 202069). Upon the writing of this report, we are aware that fewer 911 calls were made in Missoula County during 2020 (101,163) than during any of the previous three years (see Table A2 in appendix). As mentioned above, however, incidences of 911 calls in Missoula County have been declining since at least 2017, (we do not have access to data prior to 2017). So, the 2020 decrease in calls may reflect—at least in part—this broader trend. Expanding the analysis to include additional years would help mediate pandemic-related effects and increase the reliability and validity of our findings.
Lastly, we recognize that using 911 calls as a dependent variable to indicate health vulnerabilities might exclude populations that do not call emergency services for various reasons (Desmond et al., 201670). Therefore, 911 calls are not a perfect metric for uncovering public health emergency needs. Future research should investigate ways to address this potential bias.
Future Research Directions
Our future research will build on the existing analysis by adding additional time-series temperature, air quality, and 911 call data into the model. We will undertake a deeper analysis of call type and responding agency to parse out the impact of temperature and air quality events on specific incidents and, as such, community resources. In fact, this study of a single year was conducted as a proof of concept for a larger, longitudinal collaborative project. As an important first step, this study has identified, secured, and built a dataset for future research.
Future efforts will expand the number of years included in the analysis, test whether our findings on PM2.5 hold. Interestingly, our analysis finds an unexpected negative association between daily 911 calls and poor air quality days. We anticipate that including additional years of data in future analysis, particularly those with significantly worse local or western wildfire events, may uncover different (potentially positive) associations between air quality and 911 calls. In addition, we are interested in incorporating other weather events beyond high heat days (e.g., cold snaps). We expect that a time-series analysis could demonstrate whether these trends hold over multiple years, and whether there might be other factors that influence the likelihood of needing to deploy emergency resources across our community, such as the impacts of longer-term heat waves and cold snaps, or prolonged poor air quality events. Future directions could explore how data may be updated in a public, real-time dashboard and serve an important public health surveillance role.
Furthermore, the research team will further investigate the type of calls made during heat and poor air quality events. There are more than 100 call types available to 911 operators in Missoula County. We plan to employ a data reduction scheme to categorize these data with the intent to uncover whether temperature and air quality events affect certain types of emergency calls (e.g., welfare check, advanced life support). With our partners at the Center for Population Health Research, we also plan to explore how mental health as operationalized by calls for emergency evaluations (911) or helpline (988) is influenced by climate events.
Finally, because this study was designed specifically to inform public health and emergency managers in a single western Montana county, future work should explore how the findings presented above may be informative for other western rural geographies.
Acknowledgments. The authors would like to thank the exceptional public service professionals at the Missoula County Office of Emergency Management and the Missoula City-County Health Department, as well as our friends and collaborators at the University of Montana’s Center for Population Health Research (CPHR). We would not have been able to undertake this project without your support and we applaud your outstanding effort to keep our community healthy.
References
-
Campbell, S. L., Remenyi, T., & Johnston, F. H. (2023). Methods of assessing health care costs in a changing climate: A case study of heatwaves and ambulance dispatches in Tasmania, Australia. GeoHealth, 7(10), e2023GH000914. https://doi.org/10.1029/2023GH000914 ↩
-
Caulkins, M. M., Isaksen, T. B., Stubbs, B. A., Yost, M. G., & Fenske, R. A. (2016). Impacts of extreme heat on emergency medical service calls in King County, Washington, 2007-2012: Relative risk and time series analyses of basic and advanced life support. Environmental Health, 15(13), 1-13. https://doi.org/10.1186/s12940-016-0109-0 ↩
-
Wang, Q., He, Y., Hajat, S., Cheng, J., Xu, Z., Hu, W., Ma, W., & Huang, C. (2021). Temperature-sensitive morbidity indicator: Consequence from the increased ambulance dispatches associated with heat and cold exposure. International Journal of Biometeorology, 65, 1871-1880. https://doi.org/10.1007/s00484-021-02143-8 ↩
-
Austin, E., Kasner, E., Seto, E., & Spector, J. (2021). Combined burden of heat and particulate matter air quality in WA agriculture. Journal of Agromedicine, 26(1), 18-27. https://doi.org/10.1080/1059924X.2020.1795032 ↩
-
Lal, P.; Alavalapati, J.R.R.; Mercer, E.D. (2011). Socio-economic impacts of climate change on rural United States. Mitigation and Adaptation Strategies for Global Change, 16, 819–844. https://doi.org/10.1007/s11027-011-9295-9 ↩
-
Olshansky, S. J., Antonucci, T., Berkman, L., Binstock, R. H., Boersch-Supan, A., Cacioppo, J. T., ... & Rowe, J. (2012). Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Affairs, 31(8), 1803-1813. https://doi.org/10.1377/hlthaff.2011.0746 ↩
-
Jerolleman, A. (2020). Challenges of post-disaster recovery in rural areas. In S. Laska (Ed.), Louisiana’s Response to Extreme Weather: A Coastal State’s Adaptation Challenges and Successes (pp. 285-313). Springer Cham. ↩
-
Manuele, K., & Haggerty, M. (2022). How FEMA can build rural resilience through disaster preparedness. Center for American Progress. https://www.americanprogress.org/article/how-fema-can-build-rural-resilience-through-disaster-preparedness/ ↩
-
Moulton A. D. & Schramm P. J. (2017). Climate change and public health surveillance: Toward a comprehensive strategy. Journal of Public Health Management Practice, 23(6), 618-626. https://doi.org/10.1097/PHH.0000000000000550 ↩
-
Mahmood J. & Guinto R. R. (2022). Impacts of climate change on human health: Emerging evidence and call to action. Malaysian Journal of Medical Science, 29(5), 1-4. https://doi.org/10.21315/mjms2022.29.5.1 ↩
-
Bassil, K. L., Cole, D. C., Moineddin, R., Gournis, E., Schwartz, B., Craig, A. M., ... & Rea, E. (2008). Development of a surveillance case definition for heat-related illness using 911 medical dispatch data. Canadian Journal of Public Health, 99, 339-343. https://doi.org/10.1007/BF03403768 ↩
-
Portier, C. J., Tart, K. T., Carter, S. R., Dilworth, C. H., Grambsch, A. E., Gohlke, J., Hess, J., Howard, S. N., Luber, G., Lutz, J. T., Maslak, T., Prudent, N., Radtke, M., Rosenthal, J.P., Rowles, T., Sandifer, P. A., Scheraga, J., Schramm, P. J., Strickman, D., Trtanj, J. M., & Whung, P.-Y. (2013). A human health perspective on climate change: A report outlining the research needs on the human health effects of climate change. Journal of Current Issues in Globalization, 6(4), 621-710. ↩
-
Reid, C. E., & Maestas, M. M. (2019). Wildfire smoke exposure under climate change: impact on respiratory health of affected communities. Current Opinion in Pulmonary Medicine, 25(2), 179. https://doi.org/10.1097/MCP.0000000000000552 ↩
-
Conti, S., Meli, P., Minelli, G., Solimini, R., Toccaceli, V., Vichi, M., Beltrano, C., & Perini, L. (2005). Epidemiologic study of mortality during the Summer 2003 heat wave in Italy. Environmental Research, 98(3), 390-399. https://doi.org/10.1016/j.envres.2004.10.009 ↩
-
Lim, J., & Skidmore, M. (2020). Heat vulnerability and heat island mitigation in the United States. Atmosphere, 11(6), 558. https://doi.org/10.3390/atmos11060558 ↩
-
Medina-Ramón, M., Zanobetti, A., Cavanagh, D. P., & Schwartz, J. (2006). Extreme temperatures and mortality: assessing effect modification by personal characteristics and specific cause of death in a multi-city case-only analysis. Environmental health perspectives, 114(9), 1331-1336. https://doi.org/10.1289/ehp.9074 ↩
-
Klinenberg, E. (2015). Heat wave: A social autopsy of disaster in Chicago (2nd Ed.). University of Chicago Press. ↩
-
Zottarelli, L. K., Sharif, H. O., Xu, X., & Sunil, T. S. (2021). Effects of social vulnerability and heat index on emergency medical service incidents in San Antonio, Texas, in 2018. Journal of Epidemiology and Community Health, 75(3), 271-276. http://doi.org/10.1136/jech-2019-213256 ↩
-
King County Executive. (2021, June 23). Results of heat mapping project show inequitable impact of hotter summers, will inform actions by King County and City of Seattle. https://kingcounty.gov/en/legacy/elected/executive/constantine/news/release/2021/june/23-heat-mapping-results ↩
-
Lowe, D., Ebi, K. L., & Forsberg, B. (2011). Heatwave early warning systems and adaptation advice to reduce human health consequences of heatwaves. International Journal of Environmental Research and Public Health, 8, 4623-4648. https://doi.org/10.3390/ijerph8124623 ↩
-
MacMillian, C. (2023, June 28). How bad is wildfire smoke for your health? Yale Medicine. https://www.yalemedicine.org/news/how-bad-is-wildfire-smoke-for-your-health ↩
-
Weinberger, K. R., Zanobetti, A., Schwartz, J., & Wellenius, G. A. (2018). Effectiveness of National Weather Service heat alerts in preventing mortality in 20 US cities. Environment International, 116, 30-38. https://doi.org/10.1016/j.envint.2018.03.028 ↩
-
Alessandrini, E., Sajani, S. Z., Scotto, F., Miglio, R., Marchesi, S., & Lauriola, P. (2011). Emergency ambulance dispatches and apparent temperature: A time series analysis in Emilia–Romagna, Italy. Environmental Research, 111(8), 1192-1200. https://doi.org/10.1016/j.envres.2011.07.005 ↩
-
Elliot, A. J., Smith, S., Dobney, A., Thornes, J., Smith, G. E., & Vardoulakis, S. (2016). Monitoring the effect of air pollution episodes on health care consultations and ambulance call-outs in England during March/April 2014: A retrospective observational analysis. Environmental Pollution, 214, 903-911. https://doi.org/10.1016/j.envpol.2016.04.026 ↩
-
Ito, Y., Akahane, M., & Imamura, T. (2018). Impact of temperature in summer on emergency transportation for heat-related diseases in Japan. Chinese Medical Journal, 131(5), 574-582. https//doi.org/10.4103/0366-6999.226061 ↩
-
Schaffer, A., Muscatello, D., Broome, R., Corbett, S., & Smith, W. (2012). Emergency department visits, ambulance calls, and mortality associated with an exceptional heat wave in Sydney, Australia, 2011: A time-series analysis. Environmental Health, 11(3). https://doi.org/10.1186/1476-069X-11-3 ↩
-
Schneider, P., Thieken, A., & Walz, A. (2023). Effects of temperature and air pollution on emergency ambulance dispatches: a time series analysis in a medium-sized city in Germany. Weather, Climate, and Society, 15(3), 665-676. https://doi.org/10.1175/WCAS-D-22-0046.1 ↩
-
Li, Y. H., Ye, D. X., Liu, Y., Li, N., Meng, C. S., Wang, Y., ... & Yao, X. Y. (2021). Association of heat exposure and emergency ambulance calls: A multi-city study. Advances in Climate Change Research, 12(5), 619-627. https://doi.org/10.1016/j.accre.2021.06.001 ↩
-
Zhou, Q., Shi, H., Wu, R., Zhu, H., Qin, C., Liang, Z., ... & Zhang, Z. (2023). Associations Between Hourly Ambient Particulate Matter Air Pollution and Ambulance Emergency Calls: Time-Stratified Case-Crossover Study. JMIR Public Health and Surveillance, 9(1), e47022. https://doi.org/10.2196/47022 ↩
-
Rotton, J., & Cohn, E. G. (2004). Outdoor temperature, climate control, and criminal assault. Environment and Behavior, 36(2), 276-306. https://doi.org/10.1177/0013916503259515 ↩
-
Williams, A. A., Allen, J. G., Catalano, P. J., Buonocore, J. J., & Spengler, J. D. (2020). The influence of heat on daily police, medical, and fire dispatches in Boston, Massachusetts: relative risk and time-series analyses. American Journal of Public Health, 110(5), 662-668. https://doi.org/10.2105/AJPH.2019.305563 ↩
-
Kipp, A., Cunsolo, A., Vodden, K., King, N., Manners, S., & Harper, S. L. (2019). At-a-glance - Climate change impacts on health and wellbeing in rural and remote regions across Canada: A synthesis of the literature. Health Promotion and Chronic Disease Prevention in Canada, 39(4), 122-126. https://doi.org/10.24095/hpcdp.39.4.02 ↩
-
Omukuti, J., Megaw, A., Barlow, M., Altink, H., & White, P. (2021). The value of secondary use of data generated by non-governmental organizations for disaster risk management research: Evidence from the Caribbean. International Journal of Disaster Risk Reduction, 56(1), 1-22. https://doi.org/10.1016/j.ijdrr.2021.102114 ↩
-
Yeager, V. A., Menachemi, N., McCormick, L. C., & Ginter, P. M. (2010). The nature of the public health emergency preparedness literature 2000-2008: A quantitative analysis. Journal of Public Health Management Practice, 16(5), 441-449. https://doi.org/10.1097/PHH.0b013e3181c33de4 ↩
-
Mayer, B. (2019). A review of the literature on community resilience and disaster recovery. Current Environmental Health Reports, 6(3), 167-173. https://doi.org/10.1007/s40572-019-00239-3 ↩
-
Hope, K. G., Merritt, T. D., Durrheim, D. N., Massey, P. D., Kohlhagen, J. K., Todd, K. W., & D’Este, C. A. (2010). Evaluating the utility of emergency department syndromic surveillance for a regional public health service. Communicable Diseases Intelligence, 34(3), 310-318. https://pubmed.ncbi.nlm.nih.gov/21090186/ ↩
-
Leonardi, G. S., Kovats, R. S., Smith, G. E., & Gerard, E. (2006). Syndromic surveillance use to detect the early effects of heat-waves: An analysis of NHS Direct data in England. Sozial- und Präventivmedizin, 51, 194-201. https://doi.org/10.1007/s00038-006-5039-0 ↩
-
Lu, J., Metzger, K., Cajigal, A., Konty, K., & Matte, T. (2007). Identifying and modeling spatial patterns of heat-related illness in New York City. Advances in Disease Surveillance, 4, 255. https://faculty.washington.edu/lober/www.isdsjournal.org/htdocs/articles/2153.pdf ↩
-
Dale, A., Wathan, J., & Higgins, V. (2008). Secondary analysis of quantitative data sources. In P. Alasuutari, L. Bickman, and J. Brannen (Eds.) The SAGE handbook of social research methods (pp. 520-535). https://doi.org/10.4135/9781446212165 ↩
-
Peek, L., Tobin, J., Adams, R. M., Wu, H., Mathews, M. C. (2020). A Framework for Convergence Research in the Hazards and Disaster Field: The Natural Hazards Engineering Research Infrastructure CONVERGE Facility. Frontiers in Built Environment, 6, 1-19. https://www.frontiersin.org/articles/10.3389/fbuil.2020.00110 ↩
-
Missoula County. (n.d.-a). About Missoula County. Retrieved May 24, 2024, from https://www.missoulacounty.us/government/about-missoula-county ↩
-
Missoula County. (n.d.-b). Rural Program. Retrieved May 24, 2024 from https://www.missoulacounty.us/government/community-development/community-justice-department/rural-program ↩
-
Missoula City-County Health Department. (2012, January 30). Missoula County Community Health Assessment 2011. https://www.naccho.org/uploads/downloadable-resources/CHA-Missoula.pdf ↩
-
U.S. Census Bureau. (n.d.-a). Quickfacts, Missoula City, Montana. Retrieved September 28, 2023, from https://www.census.gov/quickfacts/fact/table/US,missoulacitymontana/PST045222 ↩
-
Bernstein, J. (2013, July). Creating a system to record the number of children born to under-housed mothers in Toronto. The Homeless Hub. https://www.homelesshub.ca/sites/default/files/Under%20housed%20newborns2012.pdf ↩
-
Therriault, S., & Schmidt, B. (2001, Fall/Winter). Wildfire smoke: A local health department meets the challenge. Northwest Public Health Magazine. University of Washington School of Public Health. https://sph.washington.edu/sites/default/files/2023-10/nph-therriault_f2001.pdf ↩
-
Missoula County. (n.d.). Climate Ready Missoula. https://www.missoulacounty.us/government/community-development/planning-development-and-sustainability/climate-action/climate-ready-missoula ↩
-
Maneta, D., Thompson, E., Cilimburg, A., & Silverman, N. (2019, May 3). Draft vulnerability assessment. Climate Ready Communities: Building Resiliency in Missoula County. https://www.missoulaclimate.org/uploads/4/3/2/6/43267085/vulnerability_assessment_draft_5.3.2019.pdf ↩
-
Cilimburg, A., Jones, C., Klene, A., Sharma, A., Silverman, N., & Thomkins, J. (n.d.). Mapping heat vulnerability, Missoula, Montana. Thriving Earth Exchange. Retrieved May 24, 2024, from https://thrivingearthexchange.org/project/missoula-mt/ ↩ ↩
-
Maneta, D., Cilimburg, A., Jones, C., & Lauer, C. (2020). Climate Ready Missoula. https://www.climatereadymissoula.org/uploads/1/2/6/6/126687164/draftclimatereadymissoula_1.12.20.pdf ↩
-
Minnesota Pollution Control Agency (n.d.). Air quality and health. Retrieved May 24, 2024 from https://www.pca.state.mn.us/air-water-land-climate/air-quality-and-health ↩
-
Environmental Protection Agency. (n.d.-a). Wildfire Smoke and your Patient’s Health. Retrieved May 24, 2024, from https://www.epa.gov/wildfire-smoke-course/why-wildfire-smoke-health-concern ↩
-
Worden, M., Wagner, H., Hyra, A., & Wright, D. (2022). Enhancing rigor, relevance, and equity in research and evaluation through community engagement (OPRE Report 2022-88). U.S. Department of Health and Human Services, Administration for Children and Families, Office of Planning, Research, and Evaluation. https://www.acf.hhs.gov/opre/report/enhancing-rigor-relevance-and-equity-research-and-evaluation-through-community ↩
-
U.S. Census Bureau. (n.d.-b). American Community Survey (ACS). Retrieved June 19, 2024, from https://www.census.gov/programs-surveys/acs ↩
-
Landguth, E. L., Swanson, A., Holden, Z. A., Graham, J., Warren, D., & Noonan, C. (2022). Daily 1-kilometer PM2.5 maps accounting for inversion potentials for the western United States 2003-2020 [Data set]. https://doi.org/10.6084/m9.figshare.c.5562330.v1 ↩
-
Northwest Alliance for Computational Science and Engineering, PRISM Climate Group (2024). Mean temperature in recent years. [Data set]. https://prism.oregonstate.edu/recent/ ↩
-
U.S. Census Bureau. (2010). Appendix A. Geographic Terms and Concepts. 2010 Census Redistricting Data (Public Law 94-171) Summary File. https://www2.census.gov/geo/pdfs/reference/GTC_10.pdf ↩
-
National Weather Service (n.d.). Climate charts, Missoula, MT. Retrieved May 24, 2024, from https://www.weather.gov/mso/CliPlot ↩
-
Environmental Protection Agency. (n.d.-b). Particulate Matter (PM) Basics. Retrieved May 24, 2024, from https://www.epa.gov/pm-pollution/particulate-matter-pm-basics ↩
-
Climate Smart Missoula (n.d.). The Science: Climate Change, Fires, and Human Health. Montana Wildfire Smoke. Retrieved May 24, 2024, from https://www.montanawildfiresmoke.org/the-science.html ↩
-
Raudenbush, S. W., & Bryk, A. S. (2002). Hierarchical linear models: Applications and data analysis methods (2nd ed.). Sage Publications. ↩
-
Office for Human Research Protections. 45 C.F.R. §46.104 Exempt research. (2018 Requirements). Department of Health and Human Services. https://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cfr-46/common-rule-subpart-a-46104/index.html ↩
-
Hansen A., Welton-Mitchell C., Adams R. M., Evans C. M., Peek L. Public Health Implications of Hazards and Disaster Research CONVERGE Training Module. CONVERGE Training Modules. Natural Hazards Center, University of Colorado Boulder; 2022. https://converge.colorado.edu/resources/training-modules ↩
-
Bell, M. L., Gasparrini, A., & Benjamin, G. C. (2024). Climate change, extreme heat, and health. New England Journal of Medicine, 390(19), 1793-1801. https://doi.org/10.1056/NEJMra2210769 ↩
-
American Lung Association (n.d.). Montana: Missoula, State of the Air. Retrieved May 24, 2024, from https://www.lung.org/research/sota/city-rankings/states/montana/missoula ↩
-
Kovats, S. & Koppe, C. (2005). Heat waves: Past and future impacts on health. In K. L. Ebi, J. B. Smith, & I. Burton (Eds.), Integration of public health with adaptation to climate change: Lessons learned and new directions (pp. 136-160). Routledge. http://dx.doi.org/10.1201/b17008-9 ↩
-
Abrams, D. S. (2021). COVID and crime: An early empirical look. Journal of Public Economics, 194, 104344. https://doi.org/10.1016/j.jpubeco.2020.104344 ↩
-
Ashby, M. P. J. (2020). Initial evidence on the relationship between the coronavirus pandemic and crime in the United States. Crime Science, 9(6), 1-16. https://doi.org/10.1016/j.jpubeco.2020.104344 ↩
-
Bowman IV, J. H. & Gallupe, O. (2020). Has COVID-19 changed crime? Crime rates in the United States during the Pandemic. American Journal of Criminal Justice, 45, 537-545. https://doi.org/10.1007/s12103-020-09551-3 ↩
-
Desmond, M., Papachristos, A. V., & Kirk, D. S. (2016). Police Violence and Citizen Crime Reporting in the Black Community. American Sociological Review, 81(5), 857-876. https://doi.org/10.1177/0003122416663494 ↩
Barsky, C. S., McKeague, L. K., Emidy, M. B., Walters, M., Beck, A., & Chase-Begay, D. (2024). Public Health Implications of 911 Calls During Heat and Smoke Events (Natural Hazards Center Public Health Disaster Research Report Series, Report 42). Natural Hazards Center, University of Colorado Boulder. https://hazards.colorado.edu/public-health-disaster-research/public-health-implications-of-911-calls-during-heat-and-smoke-events