Dynamics of Interorganizational Risk Management Networks During the 2015 MERS Response in South Korea
Publication Date: 2015
Summary
Between May 20, 2015 and November 24, 2015 an outbreak of the Middle East Respiratory Syndrome (MERS) coronavirus in South Korea resulted in the deaths of 38 people, 186 cases of infection confirmed, and the quarantine of 17,000 people. While the Korean national government and agencies have the overall responsibility for the MERS response, it is unclear as to how the principal agency had to coordinate the joint efforts from all levels of governments. This report aims to examine the dynamics of risk management networks including public, private, and nonprofit organizations engaged in the MERS response in South Korea.
During the field work, 11 semi-structured interviews were conducted with national, regional, and local government officials to gather data about inhibiting and facilitating factors in risk communication and response systems to MERS. Following the interviews, a survey instrument was administered to 169 organizations in order to map the pattern of communication and response networks during the MERS outbreak. To determine the pattern of interorganizational risk management, this report analyzed the survey data using Exponential Random Graph Models (ERGM).
The interview results show that governmental organizations coordinating and/or supporting the outbreak response had difficulties in communicating and cooperating with other governmental organizations. That is because the risk embedded in the outbreak response was dramatically increased by the ambiguity of the nature of the infectious disease, slow information disclosure, differences in the organizational priorities, different information standards, and the limitations of the information systems. Results of the ERGM analysis indicate that the national and subnational governments are more likely to build closed-knitted structures and directly interact with high-status organizations in order to secure core information during the outbreak response.
Introduction
A response to a novel infectious disease highlights the importance of interorganizational communication. New infectious diseases, in particular, have high ambiguity and great uncertainty regarding the nature of the virus and the virus response (Ansell et al., 20101). There is typically no clear understanding about the number of the cases and the contagion path during an outbreak. Although public officials may have some understanding about the nature of the disease, they may not know the accurate path of the disease transmission and need to rely on other public organizations in other jurisdictions.
This report aims to examine the dynamics of risk management networks among public, private, and nonprofits during the 2015 MERS outbreak response in South Korea. The outbreak resulted in the quarantine of 17,000 people, 186 cases confirmed, and a death toll of 38 (Ministry of Health & Ministry, 2015a2). While the ambiguity and uncertainty associated with an infectious disease may motivate responsible governmental agencies to rely on other organizations as information sources, it is unclear as to how each level of governments and agencies communicate with each other. I conducted 11 semi-structured interviews with national, regional, and local government officials—such as national ministries and regional or local health department staff—in order to learn more about inhibiting and facilitating factors in risk communication and response systems to MERS. Following the interviews, I administered a survey to 169 organizations to gather data to map and analyze the pattern of communication networks during the outbreak response. To determine the pattern of interorganizational collaboration and networks, I analyzed the survey data using ERGM.
This report is organized as follows: First, I describe the case of the 2015 MERS outbreak. I then described my data collection activities, measurements, and methods of analysis. The next section provides the interview results and analytical results of ERGM. The final section discusses my research findings and proposes practical implications for the United States.
South Korea Mers Outbreak Response
In the summer of 2015, South Korean society suffered from a MERS outbreak. MERS is caused by a virus called MERS Coronavirus, which affects respiratory systems, such as lungs and breathing tubes. Transmitted through close contact, the common symptoms of MERS patients include severe shortness of breath, fever, and cough. Approximately thirty to forty percent of the patients who contract MERS tend to die of the virus.
The first MERS case in South Korea was reported on May 20, 2015. A 76 year-old man visited four hospitals after his business trip in the Middle East Asian countries (Ministry of Health & Welfare, 2015a2). His symptoms at the fourth hospital were reported to the South Korea Centers for Disease Control and Prevention (CDC), which is the national disease control agency. After an investigation, the South Korean government isolated the patients’ family members and 64 clinicians. The quarantine range was not comprehensive enough to protect the population with whom the first patient and then others with whom he came into contact. Moreover, the initial government response was not effective enough to control the transmission of the disease between hospital patients and visitors.
As shown in Figure 1, the continued transmission led to an increase in the number of MERS cases over time. As of July 5, 2015, the outbreak had resulted in the quarantine of approximately 17,000 people, with 186 cases confirmed as MERS infection. The MERS outbreak affected three metropolitan regions and five provinces. On July 27, 2015, experts recommended additional quarantine measures (14 days at home) to halt the further spread of the infection (World Health Organization, 20153). Ultimately, the outbreak resulted the deaths of 36 people (Ministry of Health & Welfare, 2015b4).
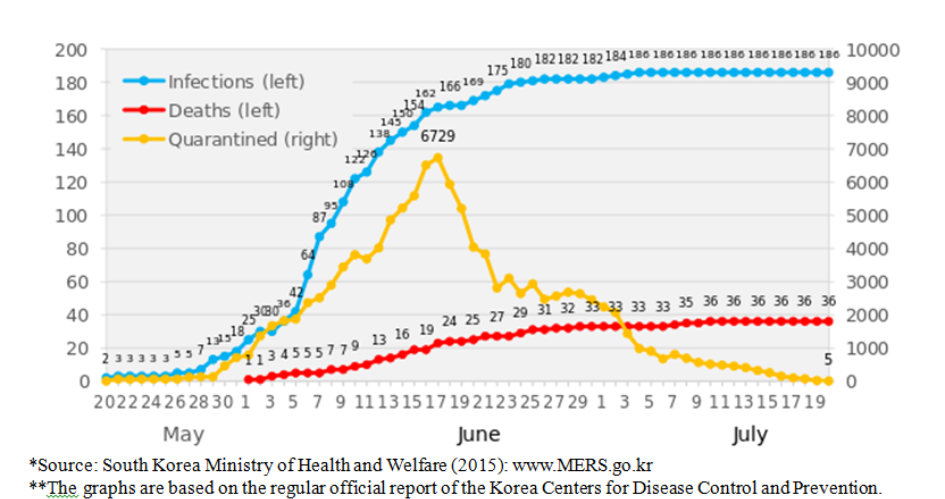 Figure 1. Trends of the MERS infection, South Korea
Figure 1. Trends of the MERS infection, South Korea
The virus response involved national agencies, regional governments, local governments, police agencies, and fire agencies. The organizations suffered from problems in risk communication. The principal national agency was reluctant to disclose the names of the hospitals that the original MERS patient visited and did not disclose this information until 17 days after the first MERS patient was identified (Ministry of Health & Welfare, 2015c5). After more people tested positive for the virus, the Ministry of Health and Welfare disclosed hospitals that had MERS patients. The Seoul Metropolitan City Government expressed dissatisfaction with the national agencies’ response actions (Ministry of Health & Welfare, 2015d6). Growing concerns about the transmission of the infectious disease highlighted both formal and informal risk communication among national and subnational governments, as well as governmental agencies that coordinate or support the outbreak response efforts.
Data And Methods
This research used a mixed methods approach with semi-structured interviews and a network survey to investigate the dynamics of interorganizational communication and collaboration during the MERS outbreak response.
Semi-Structured Interviews
I visited South Korea in January 2016 and conducted face-to-face, semi-structured interviews with public officials that were involved in the outbreak response. To learn about factors that inhibit and facilitate risk communication and response systems to MERS, I asked the following questions:
(1) Which organizations were the five most important information providers? (2) What channels did your organization use for obtaining information regarding MERS? (3) How did your organization seek and disseminate information? (4) Please rate how much your organization trusted the sources you mentioned? (5) If there was a difference in your organization’s perception of trust regarding the sources, why was this the case? (6) How did your organization disseminate this information to other organizations? (7) How did your organization disseminate this information to the residents in the jurisdiction? (8) How will your organization respond differently if another disease breaks out?
Network Survey
This report also used survey data collected from South Korea national and subnational governments in January and February 2016. I constructed a list of 169 governmental organizations: 3 ministries or national agencies, 10 regional governments or agencies, 50 district or county governments, 58 local police agencies, and 48 local fire agencies. The ministries or national agencies were responsible for coordinating or supporting the MERS outbreak response efforts at national level. The selected subnational governments and local agencies were responsible for the jurisdictions where MERS patients were identified or stayed. Subnational governments coordinated the outbreak response cooperating with regional or local agencies including local police and fire agencies. The survey was administered to the selected governmental organizations via email. In an effort to improve the response rate, I made 9-10 reminder calls. The responding organizations included 3 national ministries or agencies, 7 regional governments or agencies, 38 district or county governments, 32 local fire agencies, and 47 police agencies.
To capture the pattern of communication among the surveyed organizations, the survey asked two main questions: (1) From which organization did your organization receive information regarding MERS (e.g., patient, people under quarantine, hospital, and response) during the outbreak directly? and (2) To which organization did your organization send information regarding MERS (e.g., patient, people under quarantine, hospital, and response) during the outbreak directly? When the respondent named an organization, it was coded as ‘1’ or otherwise ‘0’. Based on the survey response, I constructed two square matrixes i.e., 169 ⅹ 169 directed matrixes that represent the observed network data (i.e., 127 survey responses) and the unobserved network data (i.e., 42 survey nonresponse).
Network Measurement
This research uses the following measures to test network and attribute effects on communicational tie formation. Governmental or nongovernmental actors develop strategies to mitigate the transaction costs in taking collective actions with other organizations under the fragmented administrative structure that lacks a chain of clear command lines (Feiock & Scholz, 20107). Emergency management organizations may take various strategies to collaborate with other organizations considering the structural relationships with other organizations (Andrew, 20108; Andrew & Carr, 20129; Jung, 201310; Jung & Song, 201511). The following network measures indicate strategies that emergency response organizations adopt in accessing core information that help the organizations to meet the needs of the target populations. The first three terms are to test whether emergency response organizations take interdependent risk management strategies or independent risk management strategies in communicating core information with other organizations.
Transitivity
The term “transitivity” represents the close relationship among three policy actors. The organizations will establish linkages to make use of local knowledge and experience and to gain associational benefits. These actions will foster trust between the organizations and will develop community strategies to address the impacts of a crisis (Pfefferbaum et al., 200512). When the focal actor (A) forms a direct tie with the actor (C) that was indirectly connected through the focal actor’s alter (B), the focal actor can create a trustworthy contact (Figure 2d). The triad structure enables the focal actor (A) to cross-check the trustworthiness of information transmitted by C through exchange with B. Transitivity is measured by geometrically weighted edgewise shared partner (GWESP), which help address a model degeneracy problem (Hunter et al., 200813).
Two-path. The term of two-path represents a relationship between two actors through one other actor i.e., an indirect relationship between A to C via B. This term is used to test the brokerage effect that represents one of the independent risk management hypotheses. When the organization collaborates with the dominant partners, it can obtain crucial information more easily and various resources that are not otherwise obtained from homogenous network members (Granovetter, 197314). When the organization takes a bridging position between the other network members that are not directly connected to each other, it can take advantage of obtaining novel information from the partners (Burt, 199415). When an actor is linked to other actors that are not otherwise connected, the actor can access novel information efficiently (Figure 2c).
Attribute effects
This term accounts for organizational type in the formation of a communication tie and is used to test the other independent risk management hypothesis. When the actor has a contact with the other actor that has a large amount of information, the former can obtain essential information without making efforts to contact other actors. When an actor is connected to a high-status actor, it can provide critical information without linking to other actors (Figure 2e). The high-status actors in the present study are national ministries or agencies and regional governments or agencies that coordinated the outbreak response at national and regional level. The dominant actors also include governmental organizations located in the Seoul metropolitan area, where the first patient and over 30 percent of the total MERS patients were identified.
This report also includes other effects for explaining the propensity for formation of a communication tie. The edge term represents the formation of an additional communication tie (Figure 2a). Because the creation of an additional tie is costly, the actor will not add a new tie unless there is a greater benefit over its cost. Reciprocity measures whether the actor establishes a tie with the other actor that has a reciprocated relationship (Figure 2b). The reciprocated relationship helps the actors develop strong commitment to each other.
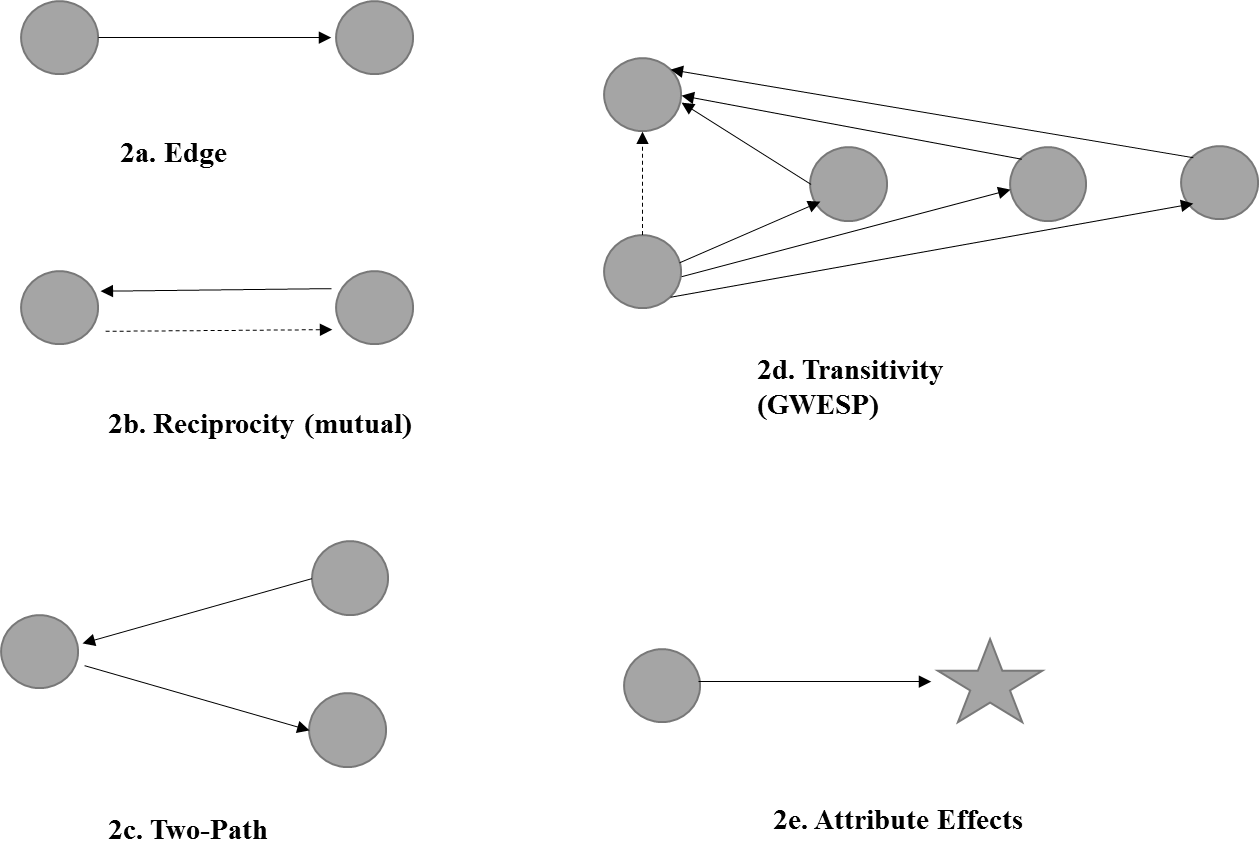 Figures 2a-2e. Network Formation
Figures 2a-2e. Network Formation
Analytical Method for Communication Tie Formation
This study employed an ERGM to analyze the pattern of the interagency risk communication network in South Korea. An ERGM allows me to analyze the observed network data with an imputation of the missing edges (i.e., survey nonresponses) (Robins et al., 200716). The study used ERGM package of statnet with R-software, which enables us to ERGM-based modeling (Hunter et al., 200813). This research establishes two models for respectively sending and receiving communication network data. The two models were converged in each of two and four iterations and produced the coefficient with high statistical significance.
Table 1 presents the summary statistics for 127 South Korean governmental organizations where there are 321 (receiving) and 255 (sending) intergovernmental ties. On average, a governmental organization communicates with 1.9 and 1.5 other governmental organizations.
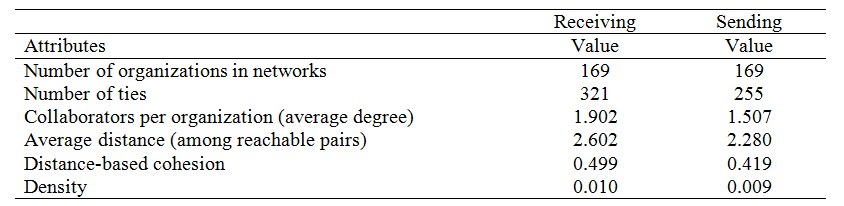 Table 1
Table 1
Results Of Semi-structured Interviews
Risk Communication
I conducted semi-structured interviews with a total of eleven public officials from four ministries, two national agencies, and five subnational governments in January 2015. I asked the interviewees regarding risk communication with governmental and non-governmental organizations and the public.
Interorganizational Risk Communication
The officials in this study reported that their organizations communicate risk information with governmental organizations, nonprofit organizations, and media. Interorganizational risk communication occurred hierarchically as well as horizontally. National agencies communicated with other national agencies or upper-level subnational governments. Lower-level subnational governments communicated risk information with national agencies or other local governments.
The interviews with local health agencies showed that communication between the local agencies and the Korean CDC officials had mixed effects on the outbreak response in the local jurisdictions. One local official reported that the Korea CDC sent its personnel to communicate directly with his local government whose jurisdiction had a MERS patient. This official said, “The CDC officials were helpful for responding to the public health jurisdiction because the national officials provided guidance to deal with the problems.” On the other hand, another local official stated that it was difficult for the local health agency to follow the guidance from CDC officials. This official said, “The national officials tried to realize the direction from the upper-level officials without considering the reality of the local response settings.”
Primary Information Channel
Government officials seemed to rely more on official government information than on media reports. The interviewees reported that national ministry and agency officials used information from the responsible ministry, agreeing that government information is usually more accurate than media coverage. National and subnational government officials reported that government information is the primary source for recognizing an outbreak problem and taking response actions. One national agency reported that the agency used media coverage to check the public perception of the agency response.
Trust of Information Sources
I asked public officials to rate the trustworthiness of the channel of information flow during the outbreak response. Their responses confirmed the differences in reliance on the information source. The interviewees rated government information as 8-10 on the-ten-point scale (with 10 being the highest level of trust) while they rated media as 3-5. Interviewees also indicated that the national government is a better channel for providing information to the governmental organizations than printed and online media. A majority of interviewees contended that media coverage focuses on the fast delivery of emergency information, sacrificing the accuracy of information. One interviewed official said, “Media may have ideological orientation and tend to report certain information without considering its trustworthiness.”
Communication with Governmental Organizations
The national and subnational governments used online and offline means to communicate with external organizations. Most interviewees reported that their organizations used telephone, email, and official letters to communicate risk information with various ministries and sub-national governments. Interviewees indicated that the organizations preferred telephone and email to formal paper communication for the immediate MERS outbreak response. One national agency personnel reported that the agency sent its personnel as a correspondent to the national ministry that coordinates government-wide response to facilitate communication with the national ministry.
Communication with the Public
Study participants reported that national ministries and sub-national governments mainly used press briefings, web pages, and social media to communicate the MERS outbreak response information with the general public. The national ministries shared the national level information with the public, while subnational governments provided information focused on the regional or local jurisdictions (e.g., numbers of MERS patients and people who were under quarantine in the jurisdictions).
Critical Response Problems
I asked the same interviewees to consider critical problems in the MERS outbreak response. Most interviewees pointed out that the responsible ministry did not share risk information with other ministries and sub-national governments immediately after the outbreak started.
Information Sharing
One informant reported that the sluggard action to disseminate information was due to consideration of the response measure after the information disclosure. Two other interviewees from subnational governments reported that the organizations sought information about hospitals with MERS patients before the responsible ministry disclosed information. The officials with whom I spoke reported that the slow information sharing was detrimental to preventing the spread of the virus.
Limitations of Information System
Study participants reported that the governmental organizations experienced several problems, even after the responsible ministry disclosed information about patients and the hospitals. First, two interviewees mentioned that the Public Health Information System (PHIS) used for sharing information about high-risk patients and people who contacted with MERS patients was problematic. Local- and regional-level public health agencies could not update information about people who contacted MERS-infected patients to the PHIS without reporting to the national disease control agency. Additionally, the system did not allow health agencies to input detailed information during the response period. The slow updates and limited information on the system were not helpful for sharing the outbreak information among local health agencies.
Insufficient Personnel
Two other informants reported that national and subnational governments did not have sufficient personnel to prevent the spread of the infectious disease. The national government or South Korean CDC had 34 epidemic investigators to confirm an MERS-infected case and only 2 of them had expertise in the investigation. Because the national government also did not immediately delegate the authority to confirm the virus infection of the high-risk patients to the subnational governments, the subnational governments relied on the national government that had limited expertise in confirming the virus infection. In addition— although health agencies of the local governments were to monitor people who contacted MERS-infected patients—the agencies did not have sufficient personnel to do so. The limited number of personnel hindered the immediate prevention efforts. After the subnational governments were delegated to confirm MERS infection, the governments in turn hired epidemic investigators from private sectors.
Lack of Resources
The South Korean governments had a lack of facilities to respond to the MERS outbreak. One ministry official and one subnational government official reported that the governmental organizations had problems in hospitalizing MERS-infected patients. The ministry official told that the ministry and its agencies were not able to provide adequate assistance to subnational governments that requested assistance during the initial response period because the governmental organization had limited resources to treat the members of the governmental organizations. The subnational government official mentioned that the responsible national agency did not have the capability to provide facilities for the patients, and the jurisdiction did not have designated public or private facilities to treat the MERS-infected patients. The subnational government was able to resolve the lack of the hospital facilities by forcing the other patients to leave one of the public hospital facilities and importing negative pressure beds.
Intraorganizational and Interorganizational Cooperation
South Korean governments had difficulties in intraorganizational and interorganizational cooperation during the outbreak response. One subnational government official reported that the responsible department had difficulties in obtaining important resources from other departments within the same government before the chief of the government led the outbreak response. The other departments became active in cooperating with the public health department after the chief of the government coordinated the outbreak response of the subnational government. The other subnational government official reported that the outbreak response was not systematic in cooperating with local health agencies, South Korea CDC, police authority, and fire authority. That is because those agencies have different reporting and command lines. One official from the national agency confirmed that the local agencies had difficulties in collaborating with local health agencies. The local official also explained that local governments had confusion in sharing information about the duration and termination date of quarantines because the governmental agencies did not have an information standard for reporting the quarantine start and terminate dates.
Similarly, one ministry official mentioned that the ministries had difficulties in gaining cooperation from the other ministries during the initial MERS response. The other ministries were passive in cooperating with the ministry for the outbreak response when the health ministry was coordinating the overall initial response. After the prime minister had led government-wide meetings for the outbreak response, the other ministries became more cooperative in the outbreak response. Another ministry official reported that the ministry was not able to communicate with the health ministry during the initial response period.
For a Future Virus Outbreak Response
The public officials I interviewed suggested several actions to better prepare for and respond to another virus outbreak.
Surveillance
The responsible agency should be able to immediately identify the inflow of a MERS-infected patient into the country. According to one national government official, the national agency had difficulties in confirming the virus infection of the first patient because the patient did not reveal the fact that he had traveled to Saudi Arabia where the virus originated. The national government may need to improve its capacity to monitor international travelers as they arrive through airports or seaports.
Organizational Capacity
The responsible agencies should improve their organizational capacity to prepare for future virus outbreaks. Most interviewees contended that the public health authority should have more professional epidemic investigators to identify virus infections and to prepare treatment facilities such as negative pressure beds. The interviewees also mentioned that the local health agencies need to have internal units and professional staff to respond to future outbreaks. One subnational government official argued that nation-wide exercises would help the responsible agencies to respond immediately to such a large scale emergency. More frequent nation-wide exercises would help the responsible agencies to identify gaps in their response protocols and to use this information to strengthen their capacity.
Active Cooperation
The national and subnational governments should make joint efforts to address response needs during the initial period of the response. Three interviewees from the national government highlighted active cooperation with relevant government agencies to address the lack of personnel and financial resources that the responsible ministry or agencies suffered in coordinating the outbreak response and addressing the needs in a timely manner.
Communication
Better risk communication will be critical for a timely and effective response to a future virus outbreak. Two interviewees—one from a ministry and another from a local health agency—stressed communication between governmental agencies about virus infection and quarantine efforts. One official said that the use of a standardized reporting format among different types of governmental agencies may facilitate the sharing of accurate information, thereby supporting a more immediate response to future outbreaks. Transparent information sharing among governmental agencies and the public will help to reduce the anxiety about the ambiguity of the infectious disease transmission.
Analysis Results Of ERGM
Network Structure of the South Korea MERS Outbreak Response
Figure 3 presents the network structure of interagency communication for the South Korea MERS outbreak response. A larger node indicates that the actor has a greater number of ties that send or receive information to/from the other actors. The network diagrams show that the national ministries or agency play central roles in coordinating and supporting the overall response, and local and regional governments or agencies interact with other governments and agencies.
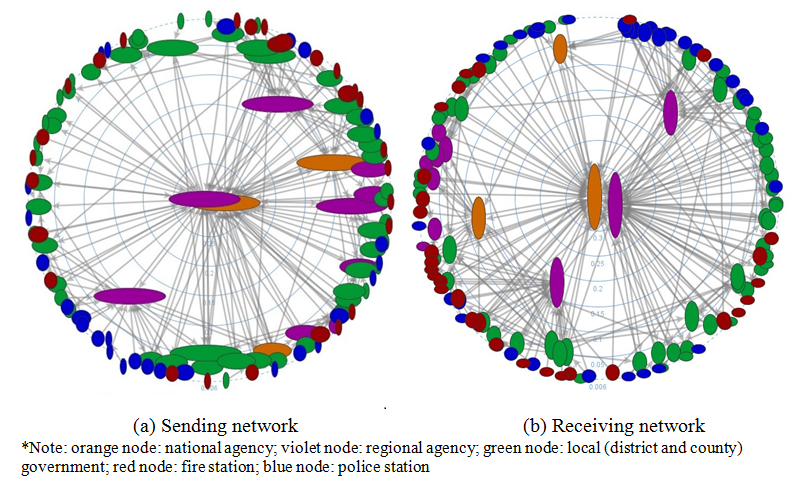 Figure 3. Interagency communication network
Figure 3. Interagency communication network
ERGM Results
Table 2 presents the ERGM results that test the structural and attribute effects on communication tie formation. Findings show positive estimates for transitivity in the two models. The coefficients are each 0.19 and 0.48, and the positive coefficients indicate that a government agency is 1.20 times (exp [0.19]) or 1.61 times (exp[0.48]) more likely to form a communication tie with an organization if the relationship has a closure structure in the network. These findings suggest that emergency response organizations may take advantage of close-knit relationships in facilitating the exchange of core information between the organizations to meet the needs of the emergency response.
While the brokerage effects are significant, the small coefficient indicates that emergency response organizations may not be actively engaged in both sending and receiving information but rather focuses on receiving information. The coefficient of two-paths is 0.02 and indicates a positive correlation between in-degree and out-degree. Because the sending model with two-paths did not converge, the brokerage effect was not included in the final model. A government agency is 1.02 times (exp [0.02]) more likely to form both a receiving tie and a sending tie, than only one type of tie. These comparatively small coefficients suggest that emergency response organizations may have difficulties in exchanging information with other organizations. An interview with a local public health official confirms the low interoperability between governmental organizations. The official reported that information exchange between cooperating governmental agencies was not smooth because of incompatibility of information sharing formats.
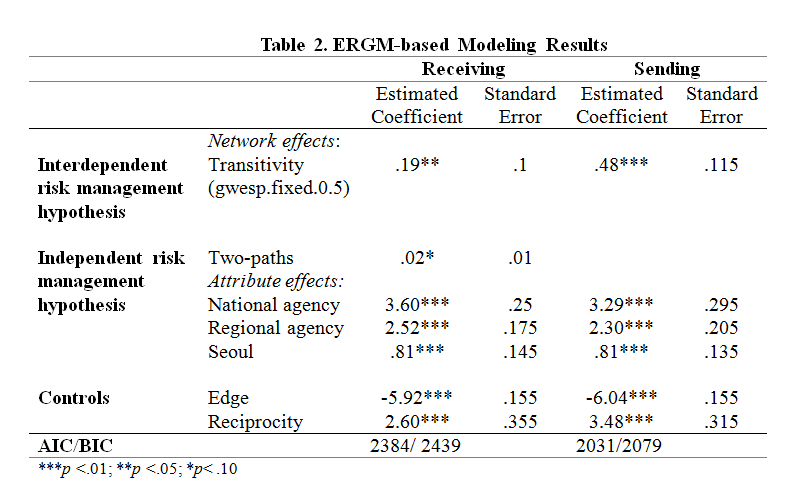 Table 2
Table 2
The attribute effects include the main effects of three types of governmental organizations: national agency, regional agency, and Seoul-based governmental organizations. The coefficients are positive in the receiving and in the sending models. The coefficients of national agency are 3.60 and 3.29 and indicate that a government organization is nearly 37 times (exp [3.60]) or 25 times (exp [3.29]) more likely to communicate with a national agency. The coefficients of regional agency are 2.52 and 2.30, showing that an emergency response organization is nearly 12 times or 10 times are more likely to communicate with a regional agency. The findings for attribute effects suggest that emergency response organizations rely heavily on the high-status organizations to obtain the core information during the national scale emergency.
The virus outbreak was not limited to one or two regions, but covers the broader areas because of the transboundary nature of the infectious disease transmission. Interviews with public health officials at regional and local governments stress the importance of transparent information sharing by the South Korean CDC and the national health ministry. The officials reported that timely information sharing by the national government would help to reduce the number of the victims.
The findings further suggest that Seoul-based governmental organizations were also important sources that provided core information for the outbreak response. The coefficients of Seoul attribute effects are both 0.81 and indicate a governmental agency is 2.2 times more likely to communicate with Seoul-based governmental agencies than with other agencies. The findings provide support for the effects of brokerage and attribute effects on the formation of a communication tie. Emergency response organizations may expect that the governmental organizations in Seoul metropolitan region would provide critical information for the outbreak response. In fact, the metropolitan region had the first MERS patients (52 patients). Because the region has nationally leading hospitals, residents from other areas came to Seoul for treatment. Visitors to the hospitals tested positive for the virus infection.
Finally, the two models have edge and reciprocity terms. The negative coefficients of edge term indicate that government organizations are less likely to form a communication tie with other organizations in general. The coefficients of reciprocity are 2.60 and 3.48 and indicate that emergency response organizations are nearly 13 times or 32 times are more likely to form a reciprocal communication ties with other organizations.
Discussion And Conclusion
Following the 2015 MERS Response in South Korea, the findings presented in this report provide key implications for theory and practice. The report identifies not only the challenges of the South Korean government’s immediate response to MERS outbreak, but also opportunities to improve the risk communication systems in managing similar kinds of diseases. The semi-structured interviews and surveys identified the obstacles blamed for slow response to the MERS outbreak. The findings of this report provide important information that highlight the need for the Korean national government and other stakeholders to take can take better protective actions in the event of a future outbreak.
In addition, this report advances understanding of how governmental organizations communicate information in responding to a public health emergency. While most of the literature to date examines who participates in a natural disaster response and which organizations play central roles in the response (e.g., Choi & Brower, 200617; Demiroz, Kapucu, & Dodson, 201218; Jung, 201310; Jung & Song, 201511; Kapucu, 200619), there is a limited understanding about what influences the interactions between emergency response organizations during a public health emergency. The findings of this report demonstrate that the systematic examination of the interactions between public organizations during the MERS response can contribute to the understanding about interorganizational communication in responding to the outbreak of an infectious disease.
Interorganizational or intergovernmental risk management is also critical for the United States in responding to the outbreak of an infectious disease. A virus outbreak is not just a problem of one jurisdiction or one region; it is of concern across multiple jurisdictions and regions. The recent outbreaks of Ebola and Zika virus in the U.S. illuminate the transboundary nature of infectious disease transmission. A 45 year-old man arrived in Dallas from Liberia transmitted Ebola virus to one of the nurses who directly cared for him. Athough Dallas was not the original site of the outbreak, the city was affected by the virus (CDC, 201420). As of March 9, 194 cases of Zika virus infection were associated with international travel while 173 cases were locally acquired. Given the latter, locally-acquired cases, there is a strong possibility that the virus may spread beyond local jurisdictions, state lines, and regions (CDC, 201420).
Since the transmission of a novel infectious disease has great uncertainty and ambiguity, public health officials should rely on officials of other jurisdictions or upper-level governments to understand the path of the virus transmission (Ansell et al., 20101). Even though public health officials did not have a virus outbreak initially in their local jurisdictions or state boundaries, their residents that traveled to the place with the outbreak can get infected. The development of transportation enables residents aggravated the transmission of an infectious disease. The transboundary nature of infectious disease transmission highlights the importance of hierarchical communication among different levels of governments, horizontal communication and cooperation between same types or different types of agencies, and information systems.
Intergovernmental Communication
All levels of governments and sectors in the United States should cooperate in sharing information regarding the transmission of an infectious disease. The findings of ERGM modeling are applicable to the intergovernmental system. To understand the overall path of the transmission in regional or national scale and to prepare for potential transmission of the jurisdiction, local public health agencies should communicate with regional government officials regarding the transmission of infectious disease, and state public health agencies should communicate with the CDC in the United States. In addition, when there are frequent travels of residents across the local jurisdictions in metropolitan areas, the local governments must communicate to each other regarding the transmission of the disease. The infection of the residents will affect people commuting from other jurisdictions. The local public health agencies from the latter jurisdictions should communicate with the former local government in identifying who the patient contacted. If the contacted residents are not monitored and infected, they may affect their family members or friends in the jurisdictions.
Interagency Communication and Cooperation
Although public health agencies are mainly responsible for responding to a virus outbreak, the response requires joint efforts from other types of agencies, such as fire agencies and police agencies. These different types of agencies may have difficulties in communicating the outbreak response. While local governments in the United States have their police departments and fire departments, there may be a still problem of collective actions among them. Because personnel from those agencies have different backgrounds of professionalization, terminology, and perspectives, they may have difficulties in communicating with each other. As one interviewee in this study reported, the agencies may not use same information standard. In normal tasks, police or fire departments communicate with the same type of agency rather than with public health departments, for example. Those agencies may not develop information standards to communicate with public health agencies unless the agencies have previous experience in doing so.
Information System
Federal governments and agencies should be able to use a disease surveillance information system effectively. The U.S. CDC operates the National Notifiable Diseases Surveillance System (NNDSS) that facilitates the exchange of public health information to public health agencies (CDC, 201521). The system provides information standards for states so that the subnational governments can share information with CDC and other health agencies. As health agencies rely more on the system, the system should be increasingly effective. CDC may need to test whether the NNDS is effective in sharing information among health agencies and the national disease control agency, regarding the transmission of the infectious disease. If the system does not update the transmission instantly, an outbreak response will be lagged and the consequence will be aggravated.
References
-
Ansell, C., Boin, A., & Keller, A. (2010). Managing transboundary crises: Identifying the building blocks of an effective response system. Journal of Contingencies and Crisis Management, 18(4), 195-207. ↩ ↩
-
Ministry of Health & Welfare (2015a). Arrival of the MERS-Infected Patient. Accessed 07 25, 2015.(http://www.mers.go.kr/mers/html/jsp/Menu_C/list_C1.jsp?menuIds=&fid=21&q_type=&q_value=&cid=62905&pageNum=1). ↩ ↩
-
World Health Organization. (2015). ‘Intensified public health measures help control MERS-CoV outbreak in the Republic of Korea’, Accessed 08 05, 2015 (http://www.wpro.who.int/mediacentre/releases/2015/20150728/en/) ↩
-
Ministry of Health & Welfare (2015b). MERS Statistics (July 28). Accessed 07 27, 2015 (http://english.mw.go.kr/front_eng/sg/ssg0111vw.jsp?PAR_MENU_ID=1001&MENU_ID=100111&page=1&CONT_SEQ=324489). ↩
-
Ministry of Health & Welfare (2015c). Hospitals with Known MERS Exposure (June, 10). Accessed 07 29, 2015. (http://english.mw.go.kr/front_eng/sg/ssg0111vw.jsp?PAR_MENU_ID=1001&MENU_ID=100111&page=1&CONT_SEQ=323285&SEARCHKEY=TITLE&SEARCHVALUE=hospital). ↩
-
Ministry of Health & Welfare (2015d). Follow-up Measure against MERS. Accessed 07 27, 2015 (http://english.mw.go.kr/front_eng/sg/ssg0111vw.jsp?PAR_MENU_ID=1001&MENU_ID=100111&page=1&CONT_SEQ=324501). ↩
-
Feiock, R. C., & Scholz, J. T. (2010). Self-organizing governance of institutional collective action dilemmas. Self-organizing federalism: Collaborative mechanisms to mitigate institutional collective action dilemmas, 3-32. ↩
-
Andrew, S. A. (2010). Adaptive versus restrictive contracts: Can they resolve different risk problems. Self-Organizing Federalism: Collaborative Mechanisms to Mitigate Institutional Collective Action Dilemmas, 91-113. ↩
-
Andrew, S. A., & Carr, J. B. (2012). Mitigating uncertainty and risk in planning for regional preparedness: The role of bonding and bridging relationships. Urban Studies, 0042098012455718. Ansell, C., Boin, A., & Keller, A. (2010). Managing transboundary crises: Identifying the building blocks of an effective response system. Journal of Contingencies and Crisis Management, 18(4), 195-207. ↩
-
[^Jung, 2013]: Jung, K. (2013). Community Resiliency and Emergency Management Networks: Following the 2012 Korean Typhoons. Natural Hazards Center (Boulder, CO), Quick Response Report QR237. ↩ ↩
-
Jung, K. & Song, M. (2015). Linking Emergency Management Networks to Disaster Resilience: Bonding and Bridging Strategy in Hierarchical or Horizontal Collaboration Networks. Quality & Quantity 49 (4): 1465-1483. DOI: 10.1007/s11135-014-0092-x. ↩ ↩
-
Pfefferbaum, B. J., Reissman, D. B., Pfefferbaum, R. L., Klomp, R. W., & Gurwitch, R. H. (2007). Building resilience to mass trauma events. In Handbook of injury and violence prevention (pp. 347-358). Springer US. ↩
-
Hunter, D. R., Handcock, M. S., Butts, C. T., Goodreau, S. M., & Morris, M. (2008). ergm: A package to fit, simulate and diagnose exponential-family models for networks. Journal of statistical software, 24(3), nihpa54860. ↩ ↩
-
Granovetter, M. S. (1973). The strength of weak ties. American journal of sociology, 1360-1380. ↩
-
Burt, R. S. (2004). Structural holes and good ideas1. American journal of sociology, 110(2), 349-399. ↩
-
Robins, G., Pattison, P., Kalish, Y., & Lusher, D. (2007). An introduction to exponential random graph (p*) models for social networks. Social networks,29(2), 173-191. ↩
-
Choi, S. O., & Brower, R. S. (2006). When practice matters more than government plans a network analysis of local emergency management. Administration & Society, 37(6), 651-678. ↩
-
Demiroz, F., Kapucu, N., & Dodson, R. (2013). 17 Community Capacity and Interorganizational Networks for Disaster Resilience. Disaster resiliency: Interdisciplinary perspectives, 334. ↩
-
Kapucu, N. (2006). Interagency communication networks during emergencies boundary spanners in multiagency coordination. The American Review of Public Administration, 36(2), 207-225. ↩
-
Centers for Disease Control and Prevention. (2014). Ebola Virus Disease Cluster in the United States — Dallas County, Texas, 2014. November 14, 2014. (http://www.cdc.gov/mmwr/preview/mmwrhtml/mm63e1114a5.htm). ↩ ↩
-
Centers for Disease Control and Prevention. (2015). National Notifiable Diseases Surveillance System (NNDSS). Accessed 03 23 2016 (https://wwwn.cdc.gov/nndss/) ↩
Kim, K. (2015). Dynamics of Interorganizational Risk Management Networks During the 2015 MERS Response in South Korea (Natural Hazards Center Quick Response Research Report Series, Report 262). Natural Hazards Center, University of Colorado Boulder. https://hazards.colorado.edu/quick-response-report/dynamics-of-interorganizational-risk-management-networks-during-the-2015-mers-response-in-south-korea