Powerless and Vulnerable: Assessing the Capacity of Elderly Healthcare Services Following Hurricane Irma
Published 2018
Abstract
Power outages following Hurricane Irma contributed to the death of at least eight Florida nursing home patients. Post-disaster power restoration is imperative to preserve the health of the elderly because they are at increased risk of heat stress and may be dependent upon life-sustaining medical equipment. This research assessed the distribution of emergency power supplies and the role of interagency connections—such as emergency management, fire safety, health care administration, and electricity provider agencies—in regulating temperatures and medical equipment at twelve nursing homes in Florida. One month after the storm, generators were documented and spatially referenced at each facility. The most recent life-safety inspection reports and consumer-friendly summaries of emergency power plans obtained from Florida’s Agency for Healthcare Administration were also examined for each nursing home. The capacity to maintain temperatures and life-sustaining equipment was not consistent within each county or between counties. Furthermore, some facilities relied on the interagency connections mentioned above to identify appropriate contractors for remediation of deficient on-site equipment to meet back-up power demands. These results establish a baseline for the improvement of onsite technology and interagency communication used to minimize future adverse health outcomes associated with extreme temperature exposure.
Introduction
Hurricane Irma made landfall in Collier County, Florida, as a Category 3 storm on September 10, 2017, and passed through Polk County, Florida, on September 11, 2017 as a Category 1 (Figure 1). Although a majority of the initial 6.5 million power outages in the state of Florida were resolved within a week of Hurricane Irma (Achenbach et al. 20171), some areas throughout the state were still without power two weeks later. Even residents that left mandatory evacuation zones for other parts of the state experienced outages after relocating. In response to post-disaster fatalities, Florida Governor Rick Scott enacted an emergency action on September 16. The action required nursing homes to comply with a specified amount of temperature-controlled space per resident and increase the duration of emergency power generation available onsite. Additionally, the order required that emergency power plans be updated to adopt changes to power supplies—such as ensuring adequate generator capacity, fuel storage, and fuel delivery arrangements—within the following sixty days (Executive Office of Governor Rick Scott 20172). This study preserves and analyzes data on the technology deficiencies that existed and the interagency connections, such as those between emergency management, health care administration, and electricity providers, that contributed to sustained healthcare provision. It also examines preparedness and response measures that influenced the poor public perceptions of nursing homes and motivated policy changes to foster proactive mitigation during recovery.
The elderly are particularly vulnerable to extreme temperature environments (Gronlund et al. 20163). Further, those reliant upon electricity to power life-sustaining equipment are at increased risk of death during power outages. Without generators to regulate temperatures and bridge power outages, the elderly experience increased vulnerability (Smith et al. 20094). Due to mobility limitations, individuals who are dependent on care may be less likely to evacuate from a hurricane. Care facilities must evacuate early and at great expense, and therefore many shelter in place (Hyer et al. 20065). Vulnerability mapping and coordination of health advocates has been identified as vital components of improving disaster outcomes for the elderly (Aldrich et al. 20086).
Electricity providers are capable of prioritizing homes and healthcare facilities that depend on life-sustaining equipment, but the extent of damages to the local infrastructure can delay such efforts (Fernandez et al. 20027). Consequently, established relationships between care providers and the larger healthcare system and those of healthcare advocates with electrical technicians can influence the likelihood of survival for the elderly (McCann 20118). The coordination between emergency management agencies, fire departments, and electrical providers to prioritize power restoration has improved emergency response, but continued success requires cross-learning (Cozzolino 20129).
Continuity is bolstered by collaboration and redundancy in post-disaster settings (Weichselgartner and Kelman 201510). The transition from relief to rehabilitation on the recovery continuum occurs approximately one month after the disaster (Paul 201111). According to Doerfel et al.’s (201012) Grounded Theory Model, this timeframe is typically between the time organizations adopt more resilient measures for future storms but before their loss of interest in adaptation.
Research Questions
This research was conducted one month after the disaster, before the improvement of emergency power supplies or interagency agreements. Nursing homes were selected from two counties in the hurricane’s path. The research questions of this study were:
What were the distribution of and potential demand for emergency power supplies that were available to nursing homes?
What is the role of existing interagency connections associated with power restoration and healthcare service provision in future heat stress mitigation efforts?
The potential heat stress and the existing processes to identify and correct safety deficiencies were analyzed. Vulnerability maps of sustainable service provision infrastructure were produced based on available networks, emergency power supplies, and population density of the elderly. Due to the time constraints of response-related research, findings established a preliminary baseline of post-disaster capacity and a framework for future research.
Methods
This research addresses gaps in the literature on the role of interagency coordination in maintaining life-sustaining medical equipment and combating heat stress for nursing home residents. The capacity to maintain life-sustaining services and combat heat stress was assessed by identifying the concentration of elderly populations, the distribution of emergency power supplies, and connectivity to interagency partners.
Area and Participant Selection
Research was conducted in Collier and Polk Counties, Florida, for comparative purposes. Although both were directly in the path of Hurricane Irma, the counties have different power companies. Electricity is primarily provided by Florida Power and Light in Collier County and Lakeland Electric in Polk County.
Two urban locations were chosen for this research: the City of Lakeland in Polk County and the City of Naples in Collier County (Figure 1).
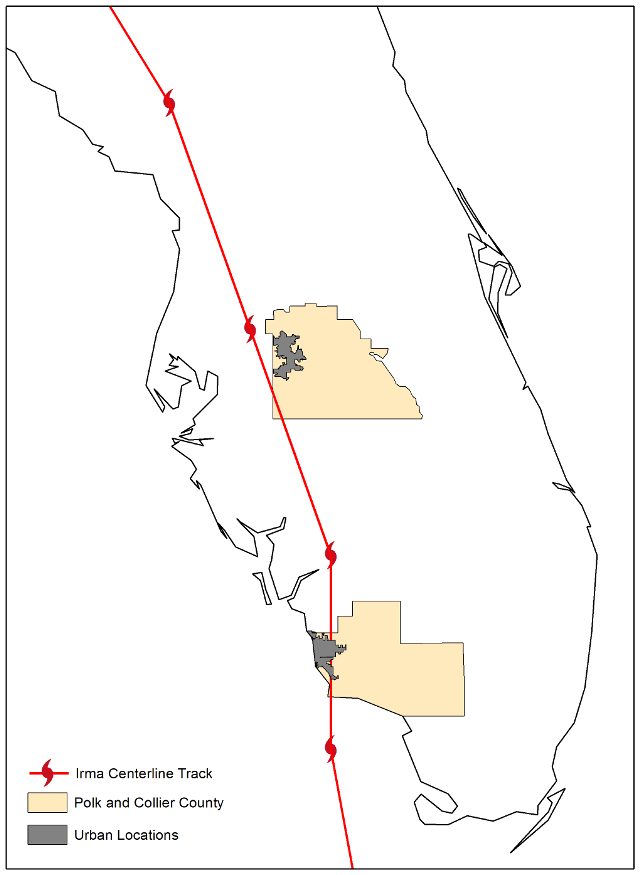
Figure 1. The track of Hurricane Irma across Florida. The field sites of Lakeland (Polk County) and Naples (Collier County) are highlighted. Source: Generated from 2010 U.S. Census TIGER/Line® files (United States Census 2012).
The population of Naples is 19,537 while Lakeland’s population is 106,420 (United States Census Bureau 201213). Approximately 20 percent of Lakeland’s population is 65 and older (Figure 2).
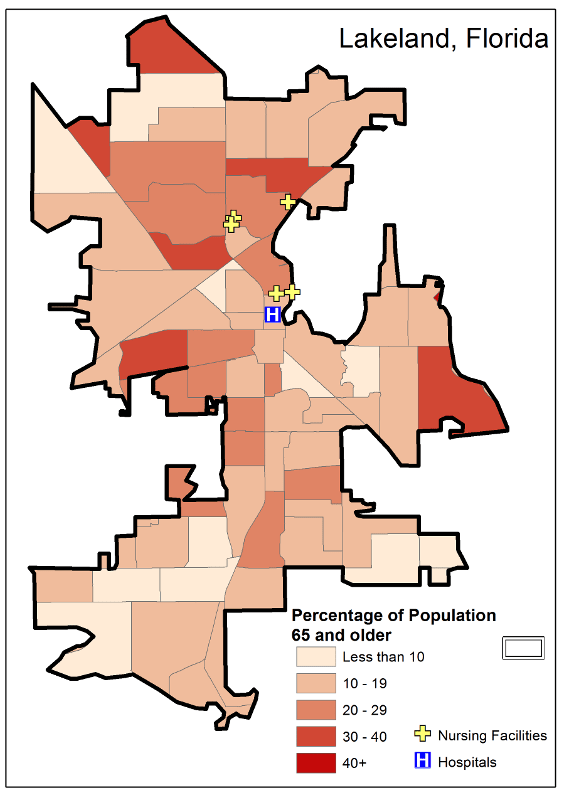
Figure 2. Lakeland, Florida, city limits. Source: Generated from 2010 U.S. Census TIGER/Line® files (United States Census 2012).
Approximately 50 percent of Naples residents are 65 or older (Figure 3).
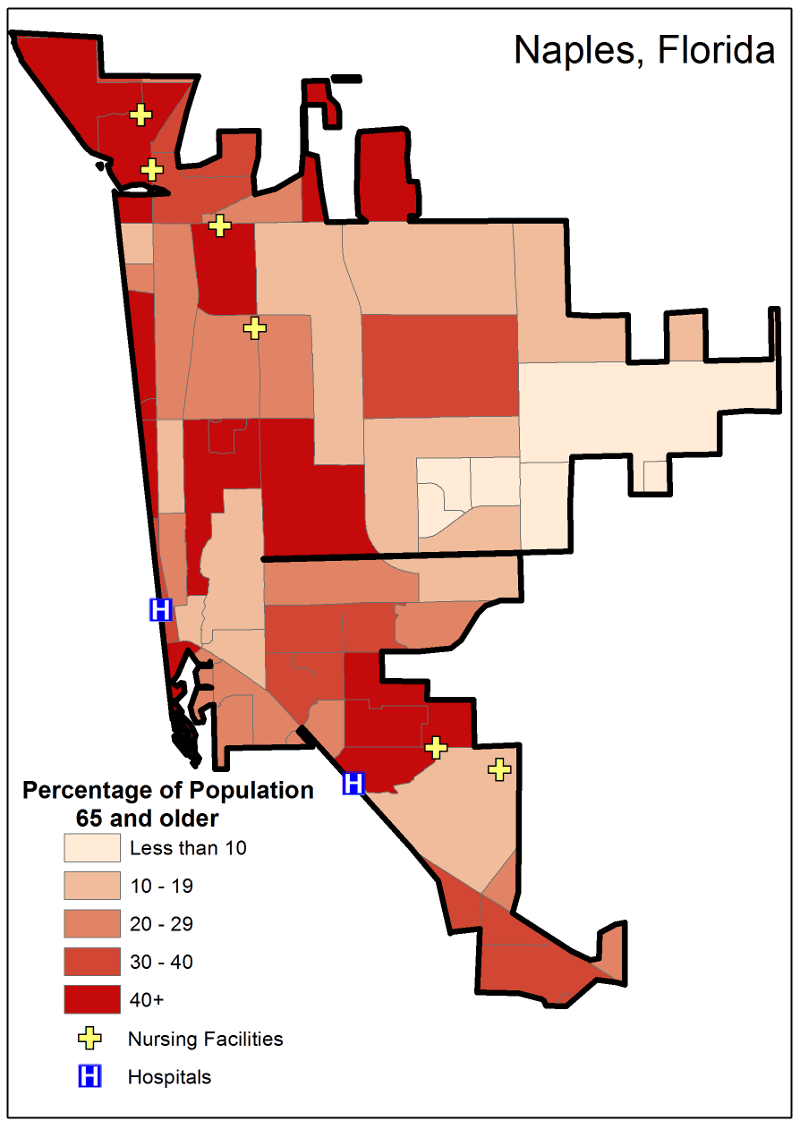
Figure 3. Naples, Florida, city limits. Source: Generated from 2010 U.S. Census TIGER/Line® files (United States Census 2012).
The Facility and Provider Locator on the FloridaHealthFinder.gov website identified 11 nursing homes in Collier County and 24 in Polk County. A total of six nursing homes from each county were included in the study. Zip codes were the most detailed level of analysis available for comparing nursing homes. Those with more than one nursing home per zip code were selected from within the Naples area, including:
(1) Harborchase of Naples and Solaris Senior Living North Naples in 34109; (2) Bentley Care Center and Solaris Healthcare Imperial in 34110; and (3) The Arlington of Naples and Manorcare of Lely Palms in 34113.
Two zip codes within Lakeland had the highest concentration of nursing homes:
(1) Consulate Health Care at Lake Parker, Lakeland Hills Center, and Lakeland Nursing and Rehabilitation in 33805; and (2) Consulate Health Care of Lakeland, The Manor at Carpenters Way, and Wedgewood Healthcare Center in 33809.
Although this is a small subset of nursing homes affected by the disaster, the range of healthcare and power infrastructure systems represented allowed for generalizations to be made about how emergency power supplies and interagency connections contribute to maintaining care.
Data Collection
On-site research was conducted on October 8 and 9, 2017—four weeks after Hurricane Irma passed through the two areas. The authors visited each accessible nursing home to document the presence of emergency power supplies externally visible to the public, using a camera that encoded geographic coordinates to each photo (photo appendices 1 and 2). One Lakeland facility and three Naples facilities could not be photographed because gates prevented entry.
The authors also obtained the most recent Florida Agency for Healthcare Administration Life-Safety Code Inspection reports and Consumer Friendly Summaries of Emergency Power Plans for each facility (Floridahealthfinder.gov 201814). Archival research of local news outlets was conducted to establish the timeframe each city was without power and associated weather data was collected from the online portal for the National Centers for Environmental Information (201715). Demographic data and hospital coordinates from the 2010 U.S. Census Bureau was mapped at the most detailed level available, the census block group, using ArcGIs 10.4.1. (ESRI 201716). Hurricane Irma’s track was outlined using data from the National Hurricane Center (2017).
Data Analysis
The progression of compliance with the governor’s emergency action was determined from the consumer friendly summaries of each nursing home’s emergency power plan, which were updated in advance of the 2018 hurricane season (Tables 1 and 2). Technological and interagency capacity to comply with fire safety requirements before the deadline were assessed from life-safety code inspection reports dated within a year of the study period. Potential heat stress and the presence of emergency power supplies to combat power failures were derived from site visits and climate data.
| Facility | Plan Approved | Date of Compliance or Expected Compliance | Emergency Power Supports | Alternate Power Source |
|---|---|---|---|---|
| Consulate Health Care at Lake Parker | 4/27/18 | 1/1/19 | AC, Life Safety Systems, Lights, Refrigeration | Fixed Generator |
| Consulate Health Care of Lakeland | 4/27/18 | 1/1/19 | AC, Life Safety Systems, Lights, Refrigeration | Fixed Generator |
| Lakeland Hills Center | 10/24/17 | 10/20/11 | Not Reported | Not Reported |
| Lakeland Nursing and Rehabilitation* | 12/12/17 | 1/1/19 | AC, Heat, Life Safety Systems, Lights, Refrigeration | Fixed and Portable Generator |
| The Manor at Carpenters | 10/24/17 | 10/4/17 | Entire Facility | Fixed Generator |
| Wedgewood Healthcare Center* | 4/27/18 | 1/1/19 | AC, Life Safety Systems, Lights, Refrigeration | Fixed Generator |
* Deficiencies reported in life safety inspection from within one year of Hurricane Irma
| Facility | Plan Approved | Date of Compliance or Expected Compliance | Emergency Power Supports | Alternate Power Source |
|---|---|---|---|---|
| Bentley Care Center | Not Reported | 12/31/18 | Life Safety Systems, Lights, Elevator, Certain Receptacles | Fixed Generator, Fuel Storage Transfer Trailer, Portable Generator |
| Harborchase of Naples* | 5/31/18 | 1/1/19 | Entire Facility | Fixed Generator |
| Manorcare at Lely Palms | 12/5/17 | 1/1/19 | Not Reported | Not Reported |
| Solaris Healthcare Imperial* | 8/1/18 | 12/31/18 | AC | Portable Generator |
| Solaris Senior Living North Naples* | 7/23/18 | 1/1/19 | AC, Lights, Refrigeration | Portable Generator |
| The Arlington of Naples, Inc. | 6/7/18 | 11/8/17 | AC, Heat, Life Safety Systems, Lights, and Refrigeration | Fixed Generator |
* Deficiencies reported in life safety inspection from within one year of Hurricane Irma
Vulnerability maps of nursing homes facilities were generated based on the proximity of the facilities to a hospital and the concentration of elderly individuals in the surrounding area (Figures 2 and 3) (Executive Office of Governor Rick Scott 2017).
Findings
Demographics
The location of nursing homes and hospitals is not consistent with a specific percentage of the elderly population. Figure 2 shows the elderly population in each nursing home’s census block group. This level of analysis provides the most detailed sample data available from the census. A block group ranges from 600 to 3,000 residents and is defined using roads, property lines, water, or other relevant boundaries. These may fall within a specific city and or zip code, which is the case in Naples and Lakeland.
The elderly population in the city of Naples was 30 percent higher than that of Lakeland ((United States Census Bureau 2012). Four of the nursing homes in Lakeland were located in census block groups with a 20 to 29 percent elderly population (Figure 2). Three of these shared the same census block group. Two of those three are operated out of the same facility. The other two nursing homes, as well as the hospital that services the city of Lakeland, share a census block group, which had 10 to 19 percent elderly population (Figure 2). Three of the nursing homes and one of the two hospitals servicing the city of Naples were located in census block groups with an elderly population of more than 40 percent (Figure 3). One of those nursing homes shared a census block group with a hospital. The other area hospital was in a census block group with a 30 to 40 percent elderly population. The three other nursing homes were in separate 30 to 40 percent, 20 to 29 percent and 10 to 19 percent elderly population census block groups (Figure 3).
Areas with the highest concentrations of elderly population, which are more vulnerable (Cutter 200617), did not align with the placement of eldercare facilities. These facilities are private or not-for-profit but all select their locations independently based on market analysis. While a higher proportion of elderly may live in a particular census block and thus increase the demand for care, the reasoning for care facility placement is beyond the scope of this study, because eligibility for admission is not restricted. However, the potential demand in the immediate vicinity and within the broader city limits could influence the capacity to provide service following the declaration of a state of emergency. A prolonged electrical outage could cause heat stress or prevent the use of life-sustaining technology in an individual’s home or at a nursing home and necessitate a search for the nearest facility to maintain that service.
Following Hurricane Irma in 2017, some care facilities experienced power outages that played a role in the deaths of at least eight elderly residents (Miller and Koh 201718). Hospitals in Lakeland and Naples are not located near the concentration of nursing homes or elderly residents, which may increase the incidence of preventable deaths if access is limited by storm related debris or roadway damage.
Temperatures
Lakeland and Naples experienced temperatures in excess of 90°F in the days following Hurricane Irma. Both locations also recorded dew points greater than 70°F. Dew point directly effects human comfort— the higher the dew point, the muggier it will feel. During episodes of extreme heat and high humidity, human thermoregulation is reduced, particularly for vulnerable populations such as the elderly. Reduced ability to cool oneself is a contributing factor to heat-related morbidity and mortality.
At Lakeland Linder Regional Airport, maximum temperatures ranged from 86 to 92°F in the days following Hurricane Irma. Dew points exceeded 70°F daily. Similarly, Naples Municipal Airport recorded temperatures between 87 and 91°F. While slightly lower than in Lakeland, Naples’ 68°F dew point coupled with the elevated maximum temperature, did not provide relief, even overnight. Lows at Lakeland did not fall below 75°F and those at Naples remained 68°F and above in the time between Hurricane Irma and full power restoration.
Rule 59A-4.1265 Emergency Environmental Control for Nursing Homes lists 81°F as the maximum temperature allowable for the temperature-controlled spaces (Agency for Health Care Administration 201719). Temperatures in Naples exceeded the maximum for 10 days and those in Lakeland for eight days before power was fully restored. Nursing homes without power would have, consequently, exceeded the maximum temperature.
Power was restored within 10 days in Lakeland and 12 days in Naples (Guinn 201720; Riley 201721). Power companies benefited from relationships with providers in other states to supplement their workforce (Harris 201722). Nursing homes and hospitals were prioritized in both locations by each county’s emergency management agency and many had power restored sooner than other businesses and residents. Not all nursing homes in these areas lost power and those that did, evern for a few hours, were able to activate existing generators.
Life-Safety Code Inspections
Life-safety code adherence in Florida nursing homes is assessed during annual unannounced inspections conducted by the fire marshal. Rule 59A-4.1265 Emergency Environmental Control for Nursing Homes was filed by the Agency for Health Care Administration (2018a23) and the Department of Elder Affairs on November 13, 2017 to make the governor’s emergency action permanent. It requires future generator maintenance checks in compliance with the Life Safety Code, Fire Prevention Code, Flammable and Combustible Liquids Code, and Standard for Liquefied Natural Gas.
Previous deficiencies could indicate the timeliness with which nursing homes might comply with the new emergency action to maintain temperatures. Further delays might stem from statewide increases in generator and fuel storage capacity, as well as the increased number of inspections needed for upgraded emergency power supplies, although the permanent legislation extended compliance deadlines to January 1, 2019 to account for strained interagency resources. Corrections in both cities required approximately one month to complete and be reinspected.
Three nursing homes in Lakeland and three in Naples did not have reported deficiencies in the year leading up to Hurricane Irma. Of the remaining three facilities in Polk County, deficiencies associated with codes pertaining to generator safety included delayed access to areas with door codes, missed fire alarm testing, and missed maintenance of fire alarms and sprinklers. External contractors were called to one facility to remediate deficiencies. Internal procedures were updated to reflect these remediation contracts and internal maintenance performed at two other facilities. At a facility shared by two healthcare providers one had deficiencies and the other did not. In the case of new power generation rules these facilities could share resources.
Deficiencies reported in Naples nursing homes included inadequate signage for fire doors, missed tests of fire detectors and sprinklers, inaccessible hallways, and failure to conduct a systems risk assessment. External contractors were called to two facilities to remediate and consult on electrical risks. Internal procedures were updated to reflect these remediation contracts. The other nursing home in Naples had not corrected the deficiencies by the date of the study, but the time limitation to do so had not expired. Although successful maintenance of life safety was not consistent within counties or even the same facility, nursing homes across the state supplemented internal capacity and comprehension of life-safety requirements through relationships with external contractors and external inspection.
Emergency Power Plans
County emergency management approves Comprehensive Emergency Plans for nursing homes and reports the date and a summary of the Emergency Power Plan portion of the comprehensive plan to the Florida Agency for Health Care Administration (2018b24) (Tables 1 and 2). Revised Emergency Power Plans were approved at two facilities in Lakeland and none in Naples by the original deadline set by the governor. By the end of 2017, one additional facility in Lakeland and one in Naples had approved plans. The remaining three facilities in Lakeland received approval in April 2018. Two additional plans were approved for Naples-based facilities by the end of May. The other three were approved after the beginning of the next hurricane season, with the last one on August 1. Plan submission was extended by the filed rule to April 2018. Further delays in approval might have occurred at the emergency management level or resulted from deficiencies.
Building plans for expanded emergency power supplies are reviewed by the Agency for Health Care Administration and inspections for compliance completed by the local fire marshal. Although the building plans are exempt public records, the compliance dates were reported in the consumer friendly summaries (Tables 1 and 2). Three facilities, one in Naples and two in Lakeland, were in compliance before the emergency action deadline. The other facilities have extensions until December 31, 2018 and January 1, 2019. All of the facilities with life-safety deficiencies from the past year had extensions for compliance (Tables 1 and 2).
Emergency Power Supplies
The nursing homes without gated entry that were publicly accessible in both countries all had visible generators. Some were on wheels for mobility, while others were not mobile. Fuel supplies and venting mechanisms were also evident at each facility. Information regarding the capacity of the generators for each facility was exempted from public record for security purposes.
A lack of deficiencies related to generators from the year before Hurricane Irma indicates that generators were up to regulatory standards for storm induced power outages, however, the amount of space cooled per resident and duration of cooling was not strictly regulated at that time. Collaborative oversight from fire marshals, county emergency management, and the Florida Agency for Health Care Administration guided the actions taken to ensure that technology was sufficient to prevent future heat-related deaths in nursing homes.
Emergency power plans detail the emergency power source and what that source will support (Tables 1 and 2). All of the facilities in Lakeland have fixed generators. Two facilities in Naples have portable generators only. One facility in each county has a combination of fixed and portable generators. One facility in each county is fully supported by emergency power. One facility in each county has a combination of fixed and portable generators. Each county had one facility where no data about the alternate power source was provided.
Although, air conditioning or spot coolers will be supported by generators under all facilities’ updated plans, only one facility in each county will be fully supported by emergency power. Heat will also be supported by emergency power supplies at one additional facility in each county. The Lakeland facilities generate power to support life- safety systems , lights, and refrigeration. In Naples life- safety systems, lights, and refrigeration will be supported at two, three, and two facilitates respectively. One Naples facility, which uses spot coolers instead of air conditioning for emergency cooling, will power specific electrical outlets during an emergency, which gives them more options for what to run in addition to the spot coolers.
Supporting refrigeration, life-safety systems, lights, and power receptacles bolsters access to care in emergencies. For example, oxygen compressors require power to receptacles and some medications, such as those for diabetes, require refrigeration. Facilities that only meet the minimum requirement to support emergency power to air conditioning systems will not receive the full benefit of life-sustaining technologies.
Recommendations and Future Research
The timely compliance with new emergency mitigation legislation is facilitated by the existing equipment and interagency collaboration available. Standards for emergency power supplies at eldercare facilities should be adopted based on potential demand for services and extreme temperature risk, and coordinated using interagency support. Locations for facilities should also consider the surrounding population and mitigation options.
To improve interagency coordination and precautionary mitigation, this study builds a baseline for future research. In addition to temperature, factors such as age, socioeconomic status, and health status have been linked to temperature-health relationships (e.g. Hajat et al. 201025; Kovats and Hajat 200826). Studies have also shown that reduced access to cooled spaces increases negative health outcomes (Eisenman et al. 201627). Additionally, similar approaches may be used for other extreme events (e.g. Abi-Samra and Malcolm 201128).
The authors plan to return to these locations to document changes in emergency power supplies, analyze life-safety records from one year after the hurricane to see how interagency relations were leveraged to maintain temperature regulating and life-sustaining equipment, and evaluate the influences of additional demographic factors on temperature-health resources. The median household income, for example, is significantly lower in Lakeland than in Naples (United States Census Bureau 2012). The extent to which this influences access to emergency power supplies requires additional research. A survey will also be conducted with nursing home managers to identify discrepancies in actual and perceived access to cooled spaces.
The study will be expanded to evaluate the emergency power plans of other elder care facilities in the southeast. Comparative studies may contribute to a framework for managing interagency connections to promote mitigation of exposure to extreme temperatures.
References
-
Achenbach, Joel, Zezima, Katie, Berman, Mark, and Wan, William. “More than 12 million without power in Florida as Hurricane Irma’s effects linger.” Washington Post, September 11, 2017. www.washingtonpost.com ↩
-
Executive Office of Governor Rick Scott. 2017. “Gov. Scott: I am aggressively fighting to keep vulnerable Floridians safe during emergencies.” Accessed December 10, 2017. https://www.flgov.com/2017/ 09/16/gov-scott-i-am-aggressively-fighting-to-keep-vulnerable-floridians-safe-during-emergencies/. ↩
-
Gronlund, Carina J., Antonella Zanobetti, Gregory A. Wellenius, Joel D. Schwartz, and Marie S. O’Neill. "Vulnerability to renal, heat and respiratory hospitalizations during extreme heat among US elderly." Climatic change 136, no. 3-4 (2016): 631-645. ↩
-
Smith, Susan M., Mary Jane Tremethick, Peggy Johnson, and June Gorski. "Disaster planning and response: considering the needs of the frail elderly." International journal of emergency management 6, no. 1 (2009): 1-13. ↩
-
Hyer, Kathryn, Lisa M. Brown, Amy Berman, and LuMarie Polivka-West. "Establishing and refining hurricane response systems for long-term care facilities." Health Affairs 25, no. 5 (2006): w407-w411. ↩
-
Aldrich, Nancy, and William F. Benson. "Peer reviewed: disaster preparedness and the chronic disease needs of vulnerable older adults." Preventing chronic disease 5, no. 1 (2008). ↩
-
Fernandez, Lauren S., Deana Byard, Chien-Chih Lin, Samuel Benson, and Joseph A. Barbera. "Frail elderly as disaster victims: emergency management strategies." Prehospital and disaster medicine 17, no. 2 (2002): 67-74. ↩
-
McCann, David GC. "A review of hurricane disaster planning for the elderly." World Medical & Health Policy 3, no. 1 (2011): 1-26. ↩
-
Cozzolino, Alessandra. Humanitarian logistics: cross-sector cooperation in disaster relief management. Springer Science & Business Media, 2012. ↩
-
Weichselgartner, Juergen, and Ilan Kelman. "Geographies of resilience: Challenges and opportunities of a descriptive concept." Progress in Human Geography 39, no. 3 (2015): 249-267. ↩
-
Paul, Bimal Kanti. Environmental hazards and disasters: contexts, perspectives and management. John Wiley & Sons, 2011. ↩
-
Doerfel, Marya L., Chih-Hui Lai, and Lisa V. Chewning. "The evolutionary role of interorganizational communication: Modeling social capital in disaster contexts." Human Communication Research 36, no. 2 (2010): 125-162. ↩
-
United States Census Bureau. 2012. “TIGER/Line Census Tracts 2010.” Accessed December 15, 2017. https://www.census .gov/geo/maps-data/data/tiger-line.html ↩
-
Floridahealthfinder.gov. 2018. “Facility/Provider Locator.” Accessed August 30, 2018. http://www.floridahealthfinder.gov/facilitylocator /FacilitySearch.aspx. ↩
-
National Hurricane Center. 2017. “Hurricane Irma.” Accessed December 10, 2017. http://www.nhc. noaa.gov/archive/2017/IRMA.shtml. ↩
-
ESRI. 2017. “New Data and Maps for ArcGIS.” Accessed December 14, 2017. http://www.esri.com/ data/data-maps. ↩
-
Cutter, Susan L. "Vulnerability to environmental hazards." Progress in human geography 20, no. 4 (1996): 529-539. ↩
-
Miller, Carol M. and Koh, Elizabeth. “Nursing home where 8 died had emergency plan with copy-paste passages, no mention of air conditioning.” Miami Herald, September 16, 2017. http://www.miamiherald.com ↩
-
Agency for Health Care Administration: State of Florida. 2017. “AHCA and DOEA Announce New Permanent Generator Rules Have Been Filed.” Accessed August 30, 2018. https://ahca. myflorida.com/Executive/Communications/Press_ Releases/pdf/ AHCAandDOEAAnnouncetheNewPermanentGeneratorRulesHaveBeenFiled.pdf. ↩
-
Guinn, Christopher. “Power Restored in Polk after Irma? It’s all in the definition.” The Ledger, September 20, 2017. http://www.theledger.com ↩
-
Riley, Patrick. “Hurricane Irma: FPL Says Some on Gulf Coast May Lack Power Until September 22.” Naples Daily News, September 12, 2017. https://www.naplesnews.com ↩
-
Harris, David. “Power restored to more than 99% of Floridians after Hurricane Irma.” Orlando Sentinel, September 20, 2017. http://www.orlandosentinel.com ↩
-
Agency for Health Care Administration: State of Florida. 2018a. “Actions to Correct Emergency Generator Problems.” Accessed August 30, 2018. https://ahca.myflorida.com/MCHQ/Plans/pdfs/Emerg_ Generator_Protocol.pdf. ↩
-
Agency for Health Care Administration: State of Florida. 2018b. “Important Tips to Ensure Safety When Using Generators.” Accessed August 30, 2018. http://ahca.myflorida.com/MCHQ/Emergency_Activities/ docs/Generator SafetyBrochure.pdf. ↩
-
Hajat, Shakoor, Madeline O'Connor, and Tom Kosatsky. "Health effects of hot weather: from awareness of risk factors to effective health protection." The Lancet 375, no. 9717 (2010): 856-863. ↩
-
Kovats, R. Sari, and Shakoor Hajat. "Heat stress and public health: a critical review." Annu. Rev. Public Health 29 (2008): 41-55. ↩
-
Eisenman, David P., Holly Wilhalme, Chi-Hong Tseng, Mikhail Chester, Paul English, Stephanie Pincetl, Andrew Fraser, Sitaram Vangala, and Satvinder K. Dhaliwal. "Heat Death Associations with the built environment, social vulnerability and their interactions with rising temperature." Health & place41 (2016): 89-99. ↩
-
Abi-Samra, Nicholas C., and Wade P. Malcolm. "Extreme weather effects on power systems." In Power and Energy Society General Meeting, 2011 IEEE, pp. 1-5. IEEE, 2011. ↩
Hutton, N. & Allen, M. (2018). Powerless and Vulnerable: Assessing the Capacity of Elderly Healthcare Services Following Hurricane Irma Natural Hazards Center Quick Response Research Report Series, Report 270). Natural Hazards Center, University of Colorado Boulder. https://hazards.colorado.edu/quick-response-report/powerless-and-vulnerable-assessing-the-capacity-of-elderly-healthcare-services-following-hurricane-irma